ALS Drug Development: A Comparative Analysis of Oral, Antioxidant, & Gene-Targeted Approaches
The development of pharmacological interventions for amyotrophic lateral sclerosis (ALS) has historically been characterized by incremental progress and limited clinical efficacy. In contrast to other neurodegenerative conditions where therapeutic diversity has expanded considerably, the ALS treatment landscape continues to rely on a small number of approved agents that confer only modest survival or functional benefits.
Nevertheless, advances in molecular genetics, cellular biology, and biomarker science have expanded the therapeutic framework and revealed multiple avenues for targeted intervention.
Contemporary ALS drug development is increasingly defined by three principal modalities: orally administered small molecules that broadly modulate neuronal excitotoxicity, antioxidant-based agents that mitigate oxidative stress, and gene-targeted therapies designed to correct or silence pathogenic mutations. Each of these approaches embodies distinct mechanistic rationales, therapeutic potentials, and translational challenges.
The following analysis examines these modalities in a comparative context, highlighting their respective advantages, limitations, and implications for the evolution of ALS therapeutics.
Oral Small Molecules in ALS
Oral small molecules represent the most traditional drug modality in ALS. These compounds are designed to modulate neuronal signaling pathways or protect against excitotoxicity. The prime example is riluzole, which inhibits glutamate release. Excessive glutamate is thought to overstimulate motor neurons, contributing to cell death.
Advantages
The appeal of oral small molecules lies in their practicality and accessibility. As drugs that can be taken by mouth, they fit seamlessly into patient care routines while maintaining a comparatively low cost of development and distribution.
- Accessibility: Oral administration makes treatment non-invasive and convenient.
- Scalability: Relatively lower cost and easier manufacturing compared to biologics or gene therapies.
- Combinability: Small molecules can be layered with other approaches, providing a therapeutic baseline for all patients.
Limitations
Despite their convenience, oral small molecules have well-recognized shortcomings. Their benefits are modest, and their mechanisms often act downstream of the core pathology, limiting overall impact.
- Modest Efficacy: Riluzole was shown to extend survival by approximately 6-19 months in real-world studies.
- Lack of Specificity: Most small molecules act downstream and are not tailored to ALS subtypes.
- Pharmacological Barriers: Blood-brain barrier penetration limits potency for many candidates.
Pipeline Examples
Ongoing research continues to expand the small molecule pipeline, aiming to refine its mechanisms and boost effectiveness.
- Riluzole Formulations: Rilutek (tablet), Tiglutik (liquid), and Exservan (oral film).
- AMX0035 (Relyvrio): A combination of sodium phenylbutyrate and taurursodiol, designed to protect mitochondria and reduce endoplasmic reticulum stress.
- Masitinib: A tyrosine kinase inhibitor under investigation for slowing functional decline.
Oral small molecules remain the most accessible ALS treatments, but their modest impact highlights the need for more advanced approaches.
Antioxidant-Based Therapies
Oxidative stress has long been implicated in ALS pathology. Reactive oxygen species (ROS) damage neurons, impair mitochondria, and accelerate degeneration. Antioxidant therapies aim to neutralize ROS and preserve motor neuron health.
Advantages
Antioxidant-based therapies are designed to address a well-established contributor to ALS pathology: oxidative damage. Their primary strength lies in targeting an aspect of the disease process that is broadly relevant across patient populations.
- Targeting a Validated Mechanism: Radicava (edaravone) showed functional benefits in ALS patients.
- Disease-Modifying Potential: While limited, these therapies slow decline by addressing oxidative damage.
- Combination-Friendly: Can be layered with oral drugs or genetic therapies.
Limitations
Despite addressing oxidative stress, antioxidant therapies are not curative. Their benefits remain supportive, and treatment administration can be more burdensome than standard oral regimens.
- Symptomatic, Not Curative: Slows progression but does not stop or reverse disease.
- Delivery Burden: Radicava initially required IV infusions; oral formulations remain more cumbersome than standard oral drugs.
- Downstream Target: Oxidative stress is a consequence of ALS, not necessarily a root cause.
Pipeline Examples
Researchers are actively exploring new antioxidants and redox-modulating agents to strengthen this modality and expand treatment choices.
- Radicava (Edaravone): FDA-approved for ALS in IV and oral forms.
- EPI-589: A novel small molecule targeting redox imbalance.
- Coenzyme Q10 Derivatives: Investigated for mitochondrial protection, though with mixed results.
Antioxidant-based strategies validate oxidative stress as a therapeutic entry point but are unlikely to be transformative alone.
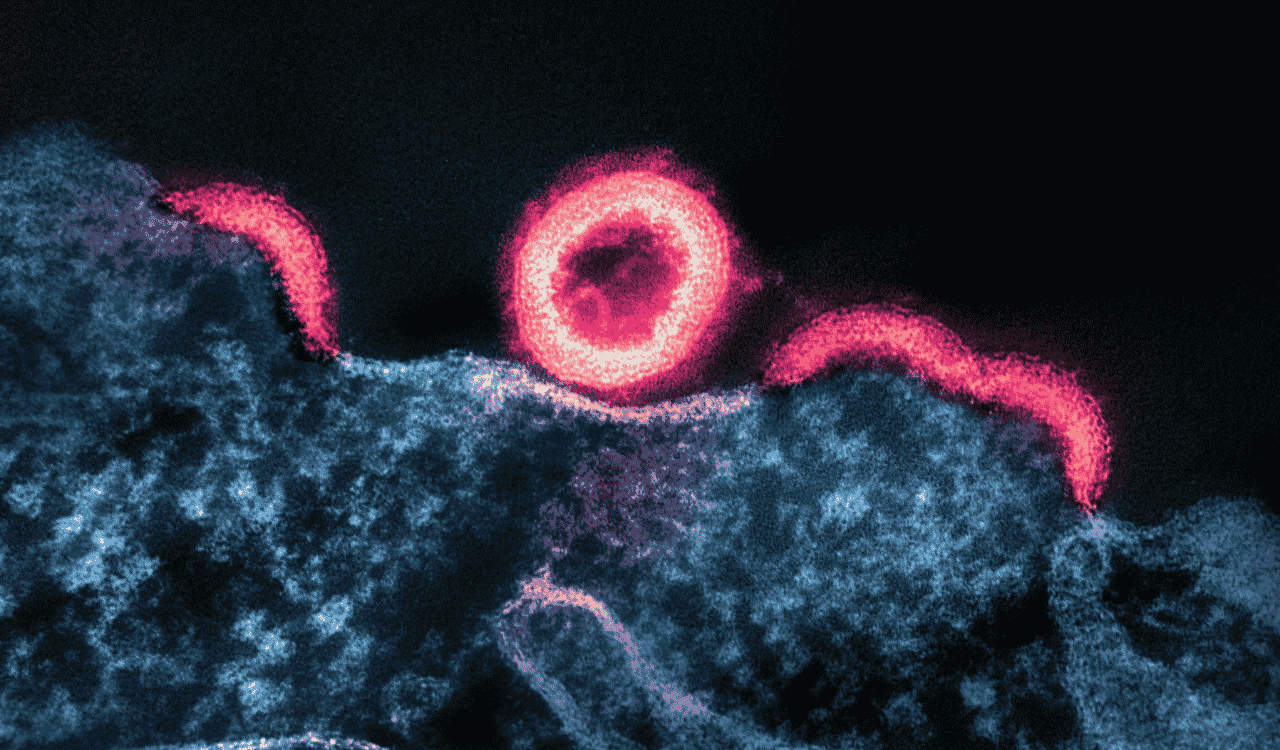
Gene-Targeted Therapies
Genetic discoveries have reshaped ALS research. Approximately 5–10% of cases are familial, with mutations in genes such as SOD1, C9orf72, FUS, and TARDBP. Gene therapies, including antisense oligonucleotides (ASOs), directly target these mutations to suppress toxic proteins or correct abnormal RNA.
Advantages
Gene therapies stand apart from traditional approaches by offering precision tools to directly address the underlying biology of ALS. Their potential impact extends beyond symptom management toward true disease modification.
- High Specificity: Designed to silence or repair causative genes.
- Disease-Modifying Potential: Unlike oral or antioxidant therapies, gene therapies can address root biology.
- Biomarker-Enabled: Advances in neurofilament light (NfL) and neuron-derived extracellular vesicles (nEVs) allow monitoring of efficacy.
Limitations
While powerful in concept, gene therapies face several real-world barriers. Their use is limited to genetically defined populations, and their delivery is invasive and costly.
- Niche Application: Only relevant for patients with defined genetic mutations.
- Delivery Challenges: Most ASOs require intrathecal injection.
- Cost and Complexity: Manufacturing and long-term safety remain significant hurdles.
Pipeline Examples
The gene therapy pipeline is one of the fastest-growing areas of ALS research, reflecting the promise of precision medicine in neurology.
- Tofersen (Qalsody): FDA-approved in 2023 for SOD1 ALS, showing biomarker reductions in neurofilament light chain.
- C9orf72 ASOs: Ongoing trials, though early results raise safety questions.
- FUS-Targeted Therapies: In preclinical or early clinical development.
Gene therapies represent a paradigm shift in ALS treatment that’s precise, biomarker-driven, and potentially transformative for subsets of patients.
Comparative Analysis: Oral vs. Antioxidant vs. Gene Therapy
When comparing these modalities, it becomes clear that each fills a different niche within the ALS treatment landscape. Evaluating their accessibility, mechanistic depth, and impact helps illustrate how they complement one another.
Accessibility vs. Precision
Oral small molecules are the most broadly accessible, while gene therapies are highly precise but limited to subsets. Antioxidants sit between the two.
Mechanistic Depth
Oral and antioxidant drugs act on downstream consequences (excitotoxicity, oxidative stress), whereas gene therapies address the root cause of pathology.
Impact & Expectations
Oral and antioxidant therapies offer modest slowing of disease progression. Gene therapies hold curative promise but only for genetically defined populations.
Practicality
Oral drugs are easiest to administer, antioxidants require more intensive dosing, and gene therapies require invasive administration and specialized infrastructure.
Future Outlook
The likely future is a layered therapeutic strategy: oral drugs and antioxidants forming a universal baseline, supplemented by gene therapy in genetically defined ALS patients.
ALS Drug Development at a Turning Point
ALS drug development is entering a new era, moving from incremental symptomatic treatments toward precision medicine. Oral small molecules and antioxidants will remain essential for broad accessibility, while gene-targeted therapies offer the most profound potential impact, even if limited to subsets of patients.
The future of ALS care is unlikely to be defined by one modality alone. Instead, progress will hinge on combination therapies, guided by biomarkers that enable patient stratification, real-time monitoring, and rapid evaluation of drug efficacy. NfL biomarkers and nEVs will be critical to making this vision a reality.
At NeuroDex, we are advancing biomarker platforms that bring unmatched specificity to ALS research. By isolating neuron-derived extracellular vesicles, our ExoSort™ technology enables the precise measurement of pathogenic proteins, including TDP-43, and supports the validation of emerging therapies. For biopharma teams and researchers, partnering with NeuroDex means gaining the clarity needed to accelerate discovery, de-risk development, and move closer to transformative treatments for ALS. Partner with us to bring greater precision to ALS drug discovery.