TDP-43 in ALS & Neurodegeneration: Key Insights
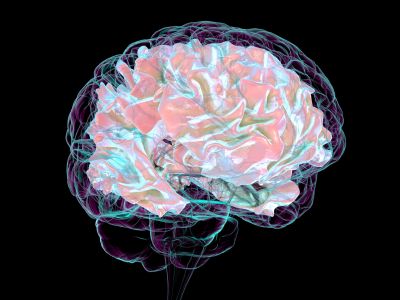
Neurodegenerative diseases are often defined by the proteins that misfold and accumulate within vulnerable neuronal populations. In Alzheimer’s disease, beta-amyloid plaques and tau tangles dominate; in Parkinson’s disease, alpha-synuclein aggregates stand out. In amyotrophic lateral sclerosis (ALS) and frontotemporal dementia (FTD), the defining culprit is TAR DNA-binding protein 43 (TDP-43).
Since its discovery in 2006 as the major component of ubiquitinated inclusions in ALS and FTD, TDP-43 has emerged as one of the most studied proteins in neurodegeneration. Pathological changes to TDP-43 — including mislocalization from the nucleus to the cytoplasm, hyperphosphorylation, truncation, and aggregation — are now recognized as a central driver of neuronal dysfunction and death. Remarkably, abnormal TDP-43 is present in about 97% of ALS cases, making it one of the most consistent molecular signatures in neurology.
Beyond ALS, TDP-43 inclusions are now identified in Alzheimer’s disease, limbic-predominant age-related TDP-43 encephalopathy (LATE), and other dementias, highlighting its broader relevance as a convergent mechanism across neurodegenerative diseases.
Explore the biology of TDP-43, how it contributes to ALS and other disorders, the challenges of measuring it in living patients, and how advances in biomarkers — particularly neuron-derived extracellular vesicles — are opening new frontiers in both research and therapeutic development.
What Is TDP-43?
TDP-43 is encoded by the TARDBP gene and belongs to the family of heterogeneous nuclear ribonucleoproteins (hnRNPs). It is a highly conserved RNA-binding protein, typically localized in the nucleus, where it regulates a wide range of RNA-related processes.
Physiological Functions of TDP-43
Under normal conditions, TDP-43 plays multiple essential roles in RNA metabolism, supporting the precise regulation of gene expression and neuronal function:
- Transcriptional Regulation: TDP-43 binds to both DNA and RNA, influencing transcriptional activity of multiple genes.
- RNA Splicing: It modulates alternative splicing of pre-mRNA, ensuring correct isoform expression of key neuronal proteins.
- mRNA Transport: In neurons, TDP-43 helps shuttle RNA transcripts into axons and dendrites, enabling local protein synthesis at synapses.
- RNA Stability: TDP-43 stabilizes certain mRNAs, protecting them from degradation.
- Stress Response: Under conditions of cellular stress, TDP-43 can transiently relocate to cytoplasmic stress granules, where it regulates translation and protects vulnerable RNAs.
These roles are critical for neuronal survival. Neurons, with their long axons and complex synaptic networks, depend heavily on finely tuned RNA metabolism. Disruptions in TDP-43, therefore, have wide-reaching consequences for cellular homeostasis.
Tight Regulation & Toxicity
One striking feature of TDP-43 biology is its requirement for precise regulation. Both overexpression and loss of TDP-43 function can be toxic. Experimental models show that too much TDP-43 impairs RNA metabolism, while depletion of TDP-43 disrupts essential splicing events and leads to cell death. This delicate balance creates a vulnerability — any pathological misregulation can quickly tip neurons into dysfunction.
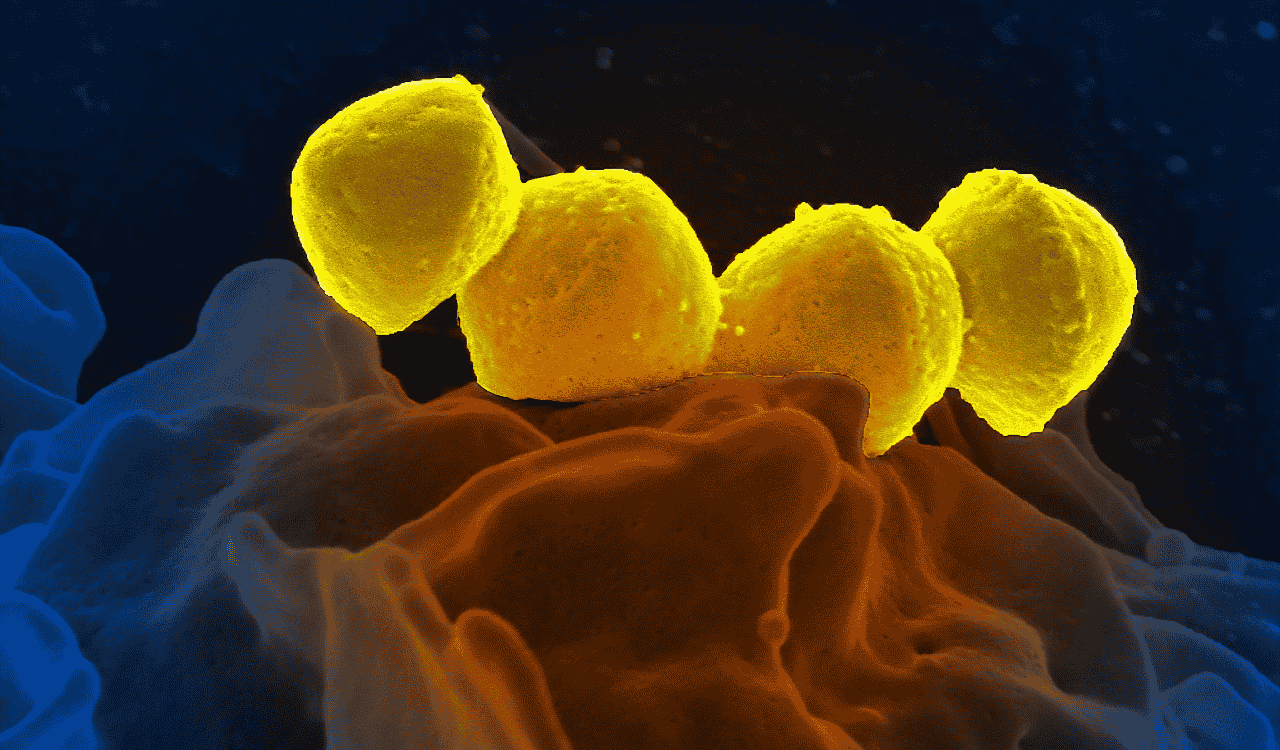
TDP-43 Pathology in ALS
TDP-43 pathology in ALS is marked by dramatic changes in localization and structure. Instead of remaining in the nucleus, where it normally resides, TDP-43 is mislocalized to the cytoplasm. There, it undergoes pathological modifications and forms insoluble inclusions.
Key Pathological Features
In ALS, TDP-43 undergoes a series of pathological changes that alter its location, structure, and function, driving widespread neuronal dysfunction:
- Nuclear Clearance: Neurons in ALS often show near-complete loss of TDP-43 from the nucleus, leading to loss of normal RNA-processing functions.
- Cytoplasmic Inclusions: Aggregated, ubiquitinated, and phosphorylated TDP-43 accumulates in cytoplasmic inclusions, which are toxic to cells.
- Truncated Fragments: Abnormal cleavage produces C-terminal fragments prone to aggregation.
- Hyperphosphorylation & Ubiquitination: Post-translational modifications exacerbate misfolding and aggregation.
Pathogenic Mechanisms
TDP-43 pathology contributes to ALS progression through a combination of mechanisms:
- Loss of Function: Depletion from the nucleus disrupts splicing and RNA stability, affecting thousands of RNA targets.
- Gain of Toxic Function: Aggregated cytoplasmic TDP-43 interferes with RNA transport, stress granule dynamics, and mitochondrial function.
- Seeding & Propagation: Evidence suggests TDP-43 aggregates may spread between neurons in a prion-like manner, contributing to disease progression.
Clinical Relevance
The near-universal presence of TDP-43 pathology in ALS makes it a defining hallmark, with only rare exceptions (e.g., patients with SOD1 or FUS mutations). This has led many to consider ALS and TDP-43 pathology almost synonymous. Its presence also explains why therapies that do not account for TDP-43 biology often fail to yield meaningful results in clinical trials.
TDP-43 Beyond ALS
While ALS remains the archetypal TDP-43 proteinopathy, its relevance extends far beyond motor neuron disease.
Frontotemporal Dementia (FTD)
A major subset of FTD cases is defined by TDP-43 pathology, with overlapping genetic and pathological features linking ALS and FTD as part of a disease spectrum. Families with C9orf72 repeat expansions often present with ALS, FTD, or both, underscoring the shared molecular underpinnings.
Alzheimer’s Disease
Up to 57% of Alzheimer’s disease (AD) cases exhibit coexisting TDP-43 pathology, particularly in limbic regions. Its presence correlates with faster cognitive decline and more severe clinical outcomes, suggesting TDP-43 may be a modifier of AD progression.
LATE (Limbic-Predominant Age-Related TDP-43 Encephalopathy)
LATE is a recently characterized disorder in older adults, mimicking Alzheimer’s clinically but pathologically driven by TDP-43 aggregation. LATE highlights the importance of recognizing TDP-43 proteinopathies as distinct disease entities.
Other Conditions
TDP-43 inclusions have been observed in subsets of Parkinson’s disease, Huntington’s disease, chronic traumatic encephalopathy, and others. This wide distribution positions TDP-43 as a unifying hallmark across neurodegeneration.
Challenges in Studying TDP-43
Despite its centrality, TDP-43 remains one of the most challenging proteins to study in living patients.
- Postmortem Reliance: For years, TDP-43 pathology could only be confirmed at autopsy, limiting translational research.
- Fluid Biomarker Difficulties: Measuring TDP-43 in cerebrospinal fluid (CSF) or blood has yielded inconsistent results. Protein fragments, low abundance, and technical variability complicate detection.
- Lack of Specificity: TDP-43 pathology occurs across multiple neurodegenerative diseases, making it harder to assign disease-specific meaning without additional context.
- Dynamic Biology: TDP-43 modifications vary by stage and disease, complicating the development of standardized assays.
This diagnostic invisibility is a major bottleneck. Without reliable biomarkers, clinical trials cannot easily stratify patients by TDP-43 pathology, nor can researchers monitor therapeutic effects targeting this protein.
Biomarkers & Advances in TDP-43 Research
Efforts to translate TDP-43 biology into measurable biomarkers are accelerating.
CSF Assays
Several groups have attempted to detect TDP-43 or its fragments in CSF, but sensitivity remains low, and results have not been widely reproducible.
Blood-Based Assays
Peripheral blood detection has also been pursued, but high background signal and low specificity to the brain limit utility.
Neurofilament vs. TDP-43
Neurofilament light chain (NfL) is currently the most validated ALS biomarker, reliably indicating neuronal injury. However, NfL reflects general neurodegeneration, not TDP-43 pathology specifically. The field now recognizes that disease-modifying therapies will require biomarkers tied directly to pathogenic proteins like TDP-43.
Neuron-Derived Extracellular Vesicles (nEVs)
A promising frontier is the use of neuron-derived extracellular vesicles — tiny particles shed by neurons into the bloodstream — as a “liquid biopsy” of the brain. Unlike total EVs or plasma proteins, nEVs carry neuron-specific cargo, including TDP-43, RNA, and metabolites. By isolating these vesicles, researchers can potentially measure TDP-43 pathology with far greater specificity, even from microliters of plasma.
If validated, nEV assays could allow real-time monitoring of TDP-43 dynamics, stratification of patients in trials, and rapid readouts of drug efficacy.
TDP-43 Therapeutic Implications
As a near-universal hallmark of ALS, TDP-43 is also a major therapeutic target. Research strategies include:
- Preventing Misfolding & Aggregation: Small molecules and antibodies designed to block pathological TDP-43 conformations.
- Enhancing Clearance: Approaches to boost autophagy and proteasome-mediated degradation of TDP-43 inclusions.
- Stabilizing RNA Metabolism: Drugs aimed at compensating for the loss of nuclear TDP-43 function.
- Gene-Targeted Therapies: Efforts to modulate upstream regulators or mutations that lead to TDP-43 pathology.
Each of these strategies will require precise biomarkers for patient selection and monitoring, highlighting again the importance of advancing detection methods.
Measuring TDP-43 with Unmatched Specificity
TDP-43 is both a hallmark and a driver of ALS and other neurodegenerative diseases. Its pathological misfolding and aggregation lead to devastating consequences for neuronal health, while its presence across disorders underscores its broader importance in neurobiology.
Yet despite this centrality, TDP-43 remains difficult to measure in living patients. Progress will depend not only on therapies aimed at its biology but also on biomarkers that make its presence visible and trackable.
At NeuroDex, we’re advancing the tools to make this possible. By isolating neuron-derived extracellular vesicles from blood, our ExoSort platform provides unmatched specificity in detecting proteins like TDP-43. For researchers and biopharma teams working to unravel ALS and related diseases, we provide the clarity needed to accelerate discovery, validate therapies, and move closer to transformative treatments.
Partner with us to unlock brain-specific biomarkers and bring the next generation of neurodegenerative therapies within reach.