
Latest Advances in Parkinson’s Clinical Trials
Parkinson’s disease is a complex neurological disorder. It affects millions worldwide, causing movement issues and tremors.
Clinical trials are crucial for developing new treatments. They help us understand the disease better.
Recent advances in Parkinson’s clinical trials are promising. Researchers are focusing on biomarkers to improve diagnosis and treatment.
A-synuclein, a protein in the brain, is a key research target. It plays a significant role in Parkinson’s pathology.
Blood biomarkers offer a non-invasive way to detect and monitor the disease. This could revolutionize early diagnosis.
Imaging techniques are advancing, helping visualize brain changes in patients. These tools enhance our understanding of the disease.
Genetic studies are paving the way for personalized medicine. They offer insights into the disease’s progression and potential treatments.
Collaboration among researchers, institutions, and patients is vital. Together, they drive progress in Parkinson’s clinical trials.
Understanding Parkinson’s Disease and the Need for Clinical Trials
Parkinson’s disease (PD) is a progressive disorder. It primarily affects motor control, leading to tremors and stiffness. As the disease advances, it may also affect cognitive functions, impacting quality of life.
The exact cause of Parkinson’s remains elusive. Both genetic and environmental factors play roles. Understanding these elements is crucial for developing effective therapies.
Clinical trials offer hope for those with PD. They test new treatments and provide insights into the disease’s progression. These trials are pivotal in finding therapies that modify disease progression rather than only addressing symptoms.
Patients with Parkinson’s can benefit greatly from clinical trial advancements. Breakthroughs in these trials could significantly improve patient outcomes.
Parkinson’s research focuses on several key areas. This includes potential new medications and strategies for early diagnosis. Furthermore, therapies that could slow or halt the progression are a priority.
For those involved, clinical trials provide several benefits:
- Access to cutting-edge treatments
- Contribution to scientific research
- Close monitoring by healthcare professionals
Participation in trials is essential for scientific progress. The involvement of patients fuels the journey toward a cure.
The global burden of Parkinson’s emphasizes the need for research. As the population ages, the number of affected individuals will rise. Thus, continuing efforts in Parkinson’s clinical trials are vital.
These trials hold promise for transformative therapies. With ongoing research and collaboration, the future of Parkinson’s treatment looks hopeful. The path to discovery continues to unfold with each scientific stride.
The Evolution of PD Clinical Trials: From Symptom Management to Disease Modification
Parkinson’s clinical trials have significantly evolved over the years. Initially, trials focused on symptom management. Medications targeted symptoms like tremors and rigidity, offering temporary relief.
As understanding of the disease improved, the focus shifted. Researchers began exploring ways to modify the disease itself. The goal became to slow or even halt progression.
Disease modification requires different strategies. Researchers now aim to address underlying causes. This involves understanding brain changes and developing innovative therapies.
Key Shifts in PD Clinical Trials:
- Symptom Management: Early focus on controlling motor symptoms.
- Disease Modification: Shift towards altering disease progression.
- Biomarker Use: Adoption of biomarkers for diagnosis and treatment efficacy.
Biomarkers have become crucial in this new era. They help stratify patients and monitor disease changes. A-synuclein, a protein involved in Parkinson’s, is a prime target in research.
The landscape of clinical trials is changing further with personalized medicine. Tailoring treatments based on individual genetic profiles promises more effective interventions. This approach could revolutionize how Parkinson’s is treated.
Collaboration is a cornerstone of progress. Research institutions, pharmaceutical companies, and advocacy groups work together. This synergy enhances clinical trial design and execution.
The integration of new technologies has also fueled advancements. Imaging technologies provide detailed insights into brain function. Digital health tools are increasingly used to track patient data in real-time.
Continuous research is vital in the fight against Parkinson’s. While many challenges remain, the trajectory is promising. The evolution from symptom management to disease modification marks a hopeful shift. As trials progress, the potential for groundbreaking therapies grows stronger.
The Role of Biomarkers in Parkinson’s Clinical Trials
Biomarkers are transforming Parkinson’s clinical trials. They provide essential insights into the disease’s progression and response to treatments. Utilizing biomarkers in trials enhances both diagnosis and patient monitoring.
Biomarkers help stratify patients into appropriate trial groups. They ensure that each group has similar disease characteristics. This increases the reliability of trial outcomes.
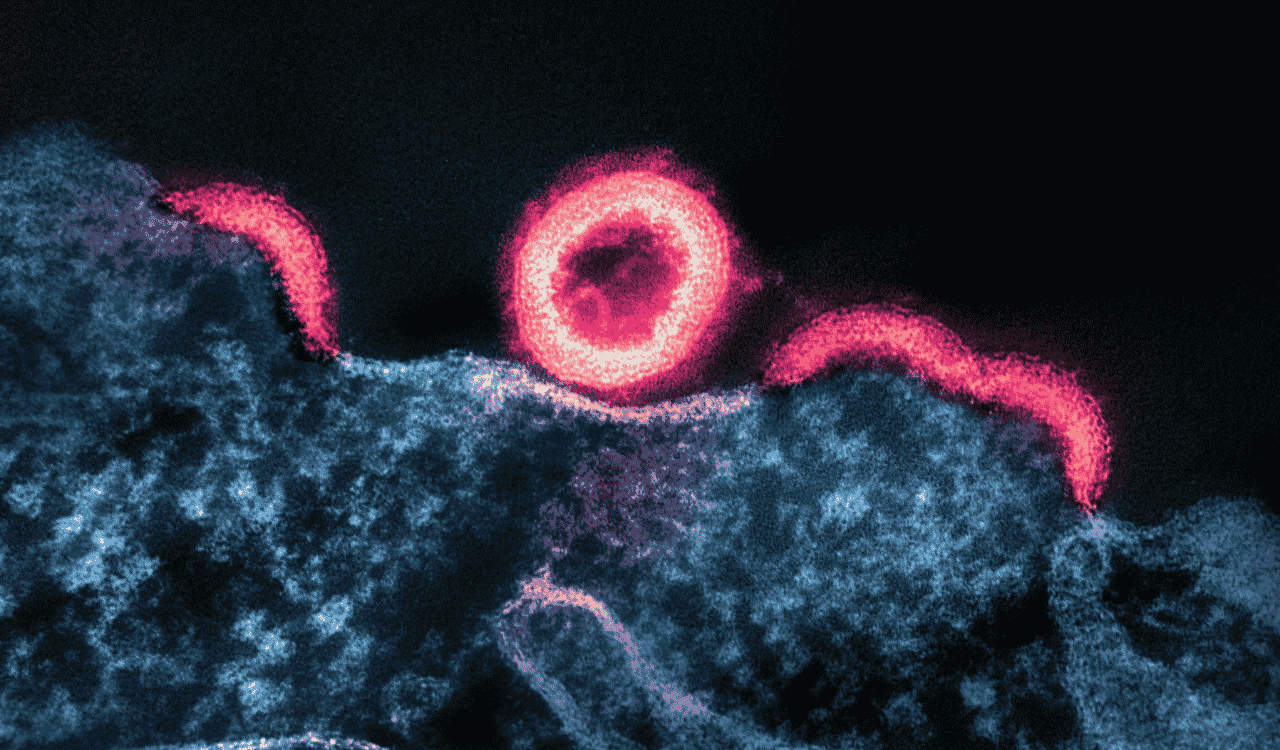
In Parkinson’s research, a-synuclein is one focal biomarker. This protein accumulates in patient brains, signifying disease presence. Its role in trials is to target this accumulation for therapeutic potential.
Blood biomarkers offer a non-invasive option. They’re used in detecting and monitoring Parkinson’s disease without invasive procedures. This ease of use makes them attractive for routine use in trials.
Important Biomarkers in Parkinson’s Trials:
- A-Synuclein: Targets protein accumulation in the brain.
- Blood Biomarkers: Non-invasive detection and monitoring tools.
- Imaging Biomarkers: Visualize structural brain changes.
Imaging biomarkers are pivotal in trials for their visual insights. They help visualize structural and functional changes in the brain.
Biomarkers can predict how a patient might respond to a treatment. They offer a personalized approach to therapy, aligning with the move towards personalized medicine in clinical trials.
Biomarker research requires collaboration across disciplines. It involves neurologists, molecular biologists, and radiologists. This collaborative effort is critical for developing robust biomarkers.
The integration of biomarkers continues to shape Parkinson’s clinical trials. They herald a new era where treatments can be more accurately designed and assessed. As research advances, biomarkers will play a greater role in improving patient outcomes.
A-Synuclein: A Key Target in Parkinson’s Research
A-synuclein is at the forefront of Parkinson’s research. It is a protein that misfolds and aggregates, a hallmark of the disease. Researchers are investigating its role as a therapeutic target.
Understanding a-synuclein is crucial. Its misfolding is linked to the degeneration of neurons. Preventing this process could slow disease progression.
Current therapies aim at reducing a-synuclein accumulation. This can potentially preserve nerve cells and their functions. Success here might revolutionize Parkinson’s treatment.
Steps in A-Synuclein Research:
- Understanding Aggregation: Study how a-synuclein aggregates in neurons.
- Developing Therapies: Create drugs targeting a-synuclein accumulation.
- Preclinical Studies: Test therapies in models before human trials.

Preclinical studies focus on assessing new therapies targeting a-synuclein. Success in these studies can lead to human trials.
Collaboration is essential in a-synuclein research. Scientists work across various fields, including biochemistry and pharmacology, to develop effective therapies.
A-synuclein research is part of broader biomarker development. It aims to create targeted therapies for Parkinson’s patients. With continued advancement, a-synuclein could be central to new Parkinson’s treatments.
Blood Biomarkers: Non-Invasive Tools for Early Detection and Monitoring
Blood biomarkers offer promise in Parkinson’s research. They are easy to collect and less invasive than other methods. This makes them ideal for repeated use in clinical trials.
Blood biomarkers can detect disease before symptoms appear. This early detection is critical for effective intervention. It allows for better timing of treatment initiation.
They help in monitoring disease progression over time. Tracking these changes is invaluable for evaluating treatment efficacy. This real-time data aids researchers in fine-tuning therapies.
Prominent Blood Biomarkers in Parkinson’s:
- Neurofilament Light Chain (NfL): Indicates neuron damage levels.
- Lipid Biomarkers: Reflect changes in brain cell membranes.
- Inflammatory Markers: Highlight active inflammation linked to progression.
Research into blood biomarkers is expanding. It involves identifying new markers and validating their clinical utility. These efforts are crucial for integrating them into routine trials.
Blood biomarkers enhance personalized medicine. They allow for treatment personalization based on individual biomarker profiles. This approach is more tailored than traditional methods.
The development and validation of blood biomarkers are ongoing. Continued innovation in this area is expected to improve Parkinson’s patient management. They represent a step forward in moving towards more non-invasive, effective clinical trials.
Recent Breakthroughs in Parkinson’s Clinical Trials
Parkinson’s research is advancing at a rapid pace. Recent breakthroughs are paving the way for new therapies. These advancements bring hope to patients and caregivers alike.
One significant area of progress is the development of disease-modifying therapies. Unlike treatments that target symptoms, these aim to slow or halt disease progression. This represents a paradigm shift in Parkinson’s therapy.
Newly discovered biomarkers are enhancing trials’ precision. They enable more accurate tracking of disease stages and treatment impacts. This improvement in trial design reduces the time needed to evaluate new therapies.
Innovative trial designs are also emerging. Adaptive trials adjust parameters based on interim results. This flexibility improves efficiency and boosts potential outcomes.
Recent Breakthroughs in Research:
- Disease-Modifying Therapies: Aiming to alter disease progression.
- Improved Biomarkers: Allowing precise tracking of therapy efficacy.
- Adaptive Trial Designs: Enhancing efficiency and outcomes.

Patient-centric approaches are gaining traction. Trials now emphasize patient-reported outcomes more than ever before. This focus ensures that patient needs are better addressed.
Collaborations between universities and the industry are increasing. These partnerships drive innovation through shared knowledge and resources. They are critical for the continued progress in Parkinson’s research.
The rise of digital health technologies is another key breakthrough. They improve patient monitoring and data collection during trials. These technologies make trials more adaptable to patient lifestyles.
Overall, recent breakthroughs are reshaping Parkinson’s clinical trials. These advances promise a brighter future for those affected by the disease.
Advances in Imaging and Digital Health Technologies
Innovations in imaging are revolutionizing Parkinson’s research. Enhanced imaging techniques reveal deeper insights into brain structure. These insights are crucial for understanding disease mechanisms.
Digital health technologies are also making waves. Wearable devices collect real-time data on patient symptoms. This information aids researchers in capturing a comprehensive patient picture.
These technologies offer several benefits. They allow continuous monitoring without hospitalization. This convenience improves patient comfort and data reliability.

Key Technologies in Parkinson’s Trials:
- Advanced Brain Imaging: Detailed views of brain changes.
- Wearable Devices: Continuous tracking of patient symptoms.
- Mobile Health Applications: Enhance patient engagement and data collection.
Mobile applications are engaging patients like never before. They enable better communication between patients and researchers. This enhances adherence to treatment protocols and trial participation.
Integration of these technologies faces challenges. Data security and patient privacy are crucial concerns. Nonetheless, these advancements hold vast potential for improving clinical trials.
Genetic Studies and Personalized Medicine in PD Clinical Trials
Genetic research is advancing our understanding of Parkinson’s. Studies uncover genetic mutations influencing disease onset and progression. These findings are pivotal for developing personalized treatment plans.
Personalized medicine tailors therapy to a patient’s genetic makeup. This approach promises greater treatment efficacy and reduced side effects. It’s increasingly becoming the focus of new PD clinical trials.
Incorporating genetic studies in trials has multiple benefits. It helps in stratifying patients based on genetic risk factors. This precision facilitates more targeted and effective trials.

Contributions of Genetic Research:
- Unveiling Genetic Mutations: Understanding mechanisms of disease onset.
- Personalized Treatments: Tailoring therapies to genetic profiles.
- Improved Patient Stratification: Enhancing trial precision and effectiveness.
The Michael J. Fox Foundation is leading in funding such studies. Their support accelerates the pace of genetic research globally. This collaboration fosters faster transition from bench to bedside.
Despite challenges, genetic studies highlight a promising future. As research continues, personalized medicine may redefine Parkinson’s treatment. The goal is to provide tailored options for each patient, marking a significant step forward in the battle against Parkinson’s.
Innovative Therapeutic Approaches: Gene Therapy, Stem Cells, and Neuroprotection
Researchers are exploring new therapeutic approaches for Parkinson’s disease. Gene therapy offers transformative potential by targeting underlying genetic causes. This approach aims to correct mutations driving the disease.
Recent trials test the safety and efficacy of gene delivery methods. These involve using vectors to introduce genetic material into brain cells. If successful, it could halt or reverse disease progression.
Stem cell therapy is another promising avenue. It involves replacing damaged neurons with healthy cells. Trials focus on ensuring these cells integrate and function properly within the brain.
One challenge is finding appropriate stem cell sources. Ethical and practical considerations drive research toward optimal solutions. These advancements hold promise for regenerating lost neural functions.
Neuroprotection strategies aim to preserve existing neurons. By preventing neuron death, these therapies can slow disease progression. Antioxidants and anti-inflammatory agents are under investigation for this purpose.
Key Innovative Approaches in Parkinson’s Therapy:
- Gene Therapy: Correcting genetic mutations.
- Stem Cell Therapy: Replacing damaged neurons.
- Neuroprotection: Preserving neuron health.
The Michael J. Fox Foundation is a key player in funding such initiatives. Their support helps researchers investigate novel therapies. This accelerates the translation of laboratory findings to clinical applications.
Collaborations with biotechnology firms facilitate these innovative trials. Such partnerships provide access to cutting-edge technology and expertise. They are crucial for overcoming technical and financial barriers.
Innovative therapies hold the promise of altering Parkinson’s treatment landscape. Each approach targets disease at a fundamental level, offering new hope. These advances represent a pivotal shift towards addressing the root causes of Parkinson’s disease.
The Importance of Patient Participation in Clinical Trials
Patient participation is vital for the success of clinical trials. Without volunteers, it’s challenging to test new treatments accurately. Patients provide real-world insights into how therapies affect them.
Participation in trials offers patients early access to cutting-edge treatments. This can be especially appealing for those with limited options. It also allows them to contribute to medical advancements that may help others.
Patient feedback during trials improves study design and outcomes. Participants provide critical data on the safety and efficacy of new interventions. This information informs future research and treatment guidelines.
Involving a diverse patient population is also essential. Diversity ensures results are applicable to different demographic groups. This leads to more personalized treatment strategies.
Benefits of Participation:
- Access to new therapies.
- Contribution to research advancements.
- Help in improving treatment strategies.
Educating patients about the trial process is crucial. Understanding study goals, risks, and benefits encourages informed participation. Clear communication ensures patients feel empowered and valued in the research process.
Patient advocacy groups play a key role in this regard. They connect patients with trial opportunities and provide support. Encouraging participation is a shared responsibility among researchers, healthcare providers, and patient communities.
Ethical Considerations and Safety in Parkinson’s Clinical Trials
Ethical standards are crucial in Parkinson’s clinical trials. Protecting patient rights ensures trust in the research process. Informed consent is a vital part, requiring clear communication about trial details.
Safety is a top priority in clinical trials. Researchers must monitor patient health vigilantly. Regular assessments help identify potential adverse effects early.
Participants should receive detailed explanations about possible risks and benefits. This knowledge allows them to make informed decisions about joining the study. Transparency throughout the trial fosters confidence and engagement.
The use of placebos in trials is carefully managed. Ethical guidelines dictate their use only when necessary. Researchers always weigh the potential benefits against possible harm.
Key Ethical Considerations:
- Informed consent process.
- Patient safety and monitoring.
- Transparent communication and risk management.
Collaborations with ethics committees ensure ongoing oversight. These committees review trial protocols to ensure ethical compliance. Their involvement helps maintain high standards and safeguards patient welfare.
Collaboration and Funding: Driving Progress in PD Research
Collaboration is the backbone of successful Parkinson’s disease research. Strong partnerships among stakeholders enable shared knowledge. These efforts enhance the development and execution of clinical trials.
Funding plays a pivotal role. It provides resources needed for cutting-edge research. Organizations like the Michael J. Fox Foundation significantly contribute to PD research funding.
Cross-institutional collaborations bring diverse expertise. Researchers, clinicians, and patients work together towards common goals. This unity accelerates the development of new therapies and innovations.
Key funding sources include:
- Non-profit organizations
- Government grants
- Pharmaceutical companies
Such funding supports a wide range of projects. It fuels studies exploring innovative treatments and technologies. Consistent funding ensures sustained progress in finding effective Parkinson’s therapies.
Collaboration with advocacy groups raises public awareness, too. These groups inspire broader support for vital research efforts. Through this collective action, the future of PD research remains bright and promising.
How to Find and Join a Parkinson’s Clinical Trial
Finding and joining a Parkinson’s clinical trial can seem overwhelming. However, numerous resources exist to guide you. With the right information, participation becomes more accessible.
Start by consulting your healthcare provider. They can provide valuable advice on suitable trials. Discuss any concerns or questions you might have.
Online platforms are invaluable, too. Websites like ClinicalTrials.gov offer detailed information. Here, you can search for trials based on location and eligibility.
When considering a trial, keep in mind:
- Eligibility criteria
- Trial location
- Duration and commitment required
- Potential risks and benefits
Joining a trial contributes significantly to research. It offers a chance to access new treatments and contribute to medical advancements. By participating, you help shape the future of Parkinson’s therapies, providing hope for many others living with the disease.
The Future of Parkinson’s Clinical Trials: Challenges and Opportunities
The path forward for Parkinson’s clinical trials is both promising and complex. Innovative strategies are addressing the disease’s diverse nature. Researchers aim to unravel its mysteries further.
Challenges arise with trial diversity and patient recruitment. Including varied populations ensures broad applicability. A focus on diversity helps create inclusive treatment options.

Opportunities abound in technological advances. Digital health tools and AI can streamline research processes. These innovations may revolutionize trial methodologies and data analysis.
Key areas for future focus include:
- Enhancing trial diversity
- Leveraging technology for better data
- Developing personalized therapies
- Increasing patient engagement
The evolving landscape of Parkinson’s trials holds immense potential. Combining cutting-edge science with broader participation can lead to breakthroughs. By tackling current challenges, the hope is to offer effective solutions for those affected by Parkinson’s, improving lives significantly.
Key Takeaways and Next Steps for Patients and Caregivers
Understanding Parkinson’s clinical trials is crucial for patients and caregivers. Staying informed helps in making educated decisions about participation and treatment options.
Engage actively with healthcare professionals. They provide insights into the latest developments and trial opportunities that might be suitable. Having open discussions can aid in managing expectations and planning effectively.
Consider the following next steps:
- Stay updated with recent research.
- Join support groups for shared experiences.
- Discuss trial options with your medical team.
Empowering oneself with knowledge and resources leads to better care management. Staying proactive ensures you can benefit from advancements in Parkinson’s research and clinical trials.


Leave a Reply