Next-Generation Biomarkers for Neurodegeneration
Biomarker Discovery News: Revolutionizing the Fight Against Neurodegenerative Diseases
The human brain, a marvel of biological engineering, is the nexus of our consciousness, memories, and very identity. Yet, this intricate organ is susceptible to a group of devastating and progressive conditions known collectively as neurodegenerative diseases. These relentless disorders, including Alzheimer’s Disease, Parkinson’s disease, frontotemporal dementia, and amyotrophic lateral sclerosis (ALS), silently erode neural function, leading to profound cognitive decline, motor impairment, and often, drastic changes in personality and behavior.
The global burden of these neurodegenerative conditions is staggering; in 2025, an estimated 7.2 million Americans aged 65 and older are projected to be living with Alzheimer’s dementia, and globally, 3.4 billion people experienced a nervous system condition in 2021, according to the Global Burden of Disease study.
The cost associated with care is equally immense, with the total cost for caring for people with Alzheimer’s and other dementias in the United States projected to reach $384 billion in 2025, as noted by the Alzheimer’s Association. In 2023 alone, Parkinson’s disease accounted for 11.67 million cases and 0.42 million deaths globally, highlighting its significant impact according to Global Burden of Disease data. These alarming statistics underscore the urgent need for advancements in diagnostics and therapeutic strategies. Fortunately, the field of biomarker discovery is experiencing an unprecedented surge in innovation, offering a beacon of hope for earlier detection, more accurate diagnoses, and the development of precision therapies for these complex neurodegenerative disorders.
The Urgent Need for Better Neurodegenerative Disease Diagnostics
The insidious nature of neurodegenerative diseases presents a formidable challenge to both patients and the healthcare system. These conditions often begin years, even decades, before clinical symptoms become apparent. This prolonged silent phase means that by the time a diagnosis is made, substantial neuronal loss has already occurred, significantly limiting the effectiveness of available interventions. The lack of sensitive and specific diagnostic tools means that many individuals receive a diagnosis only after significant irreversible damage has occurred. This delays crucial interventions and limits the potential efficacy of emerging therapies. The urgent need for better diagnostic strategies, particularly those allowing for early detection, is paramount to shifting the trajectory of these debilitating conditions. Parkinson’s disease cases, for instance, are projected to reach 25.2 million by 2050, a 112% rise from 2021, underscoring the critical need for enhanced diagnostic capabilities and care worldwide according to recent projections.
The Current Landscape of Diagnosis
Current diagnostic approaches for neurodegenerative diseases are often reactive and insufficient. Diagnosis typically relies on a combination of detailed medical history, neurological examinations, cognitive assessments, and sometimes neuroimaging techniques like MRI or PET scans. While these methods can identify the presence of disease and its severity, they often lack the specificity and sensitivity required for early and definitive diagnosis, particularly in the pre-symptomatic stages. Furthermore, some definitive diagnostic tools, such as PET scans for amyloid and tau pathology in Alzheimer’s disease, are expensive and not widely accessible. Lumbar punctures to analyze cerebrospinal fluid (CSF) are also invasive and carry their own set of risks and patient discomfort, contributing to delays in diagnosis and limited applicability for widespread screening. These inherent limitations highlight the critical need for more accessible, less invasive, and highly accurate diagnostic modalities.
The Promise of Early Detection and Precision: Why Biomarkers Matter Now
Biomarkers are measurable biological indicators that can objectively signal a particular biological state, disease process, or response to treatment. In the context of neurodegenerative diseases, biomarkers offer a revolutionary paradigm shift. They hold the potential to detect disease at its earliest stages, even before symptoms manifest, allowing for early intervention and potentially slowing or halting disease progression. Beyond diagnosis, biomarkers can help differentiate between various neurodegenerative disorders, which often present with overlapping symptoms.
This precision is crucial for tailoring treatments to the specific underlying pathology of a patient’s disease, moving away from a one-size-fits-all approach towards truly personalized medicine. Moreover, biomarkers are essential for guiding clinical trials, monitoring therapeutic responses, and enabling the development of novel therapeutic strategies.
Understanding Neurodegeneration: Key Concepts and Disease Examples (Alzheimer’s, Parkinson’s, Frontotemporal Dementia)
Neurodegeneration is a complex process characterized by the progressive loss of neuron structure or function, including their death. This loss can occur in specific brain regions, leading to distinct clinical syndromes. Alzheimer’s Disease (AD), the most common cause of dementia, is characterized by the accumulation of amyloid plaques and tau tangles, leading to widespread neuronal dysfunction and loss, primarily affecting memory and cognitive function.
These neurodegenerative conditions include Alzheimer’s Disease, Parkinson’s disease, frontotemporal dementia, and amyotrophic lateral sclerosis (ALS). They slowly damage brain function, causing serious problems with thinking, movement, and often changes in personality and behavior. Parkinson’s disease (PD) is primarily characterized by the loss of dopaminergic neurons in the substantia nigra, leading to motor symptoms such as tremors, rigidity, and bradykinesia.
Frontotemporal dementia (FTD) is a group of disorders caused by progressive nerve cell loss in the brain’s frontal lobes (behind the forehead) and temporal lobes (behind the ears), affecting personality, behavior, and language.
Amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s disease, is a progressive neurodegenerative disease that affects nerve cells in the brain and spinal cord, leading to muscle weakness, paralysis, and eventual respiratory failure. Early identification of these diseases is vital for targeted treatment.
What Are Biomarkers? Decoding the Body’s Messengers
A biomarker is a measurable trait that scientists measure and evaluate. It shows normal body processes, disease processes, or responses to treatment. In essence, they are the body’s way of signaling that something is happening internally, providing objective clues that can be detected and interpreted. For neurodegenerative diseases, biomarkers can range from specific proteins and genetic variants to imaging findings and physiological measurements. Their fundamental role is to provide an early, objective, and reliable assessment of disease state. This is critical because many neurodegenerative disorders are characterized by slow, progressive pathological changes that precede overt clinical symptoms. By identifying these underlying changes, biomarkers allow for a more proactive approach to diagnosis and management. Reliable Biomarker Testing is transforming how we understand and fight these conditions.
Defining Biological Markers and Their Role in Disease
A biological marker, or biomarker, is a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes, or pharmacologic responses to a therapeutic intervention. For neurodegenerative diseases, biomarkers can range from specific proteins and genetic variants to imaging findings and physiological measurements. Their fundamental role is to provide an early, objective, and reliable assessment of disease state. This is critical because many neurodegenerative conditions are characterized by slow, progressive pathological changes that precede overt clinical symptoms. By identifying these underlying changes, biomarkers allow for a more proactive approach to diagnosis and management.
Types of Biomarkers Revolutionizing Neurodegenerative Conditions
The field of biomarker research for neurodegenerative diseases is rapidly advancing, with significant progress across several categories. One key area is the study of specific proteins. For instance, neurofilament light (neurofilament light chain, NfL), a protein component of the neuronal cytoskeleton, is released into the bloodstream and cerebrospinal fluid when neurons are damaged. Elevated NfL levels serve as a general indicator of neuroaxonal damage, making it a valuable biomarker across various neurodegenerative conditions, including Alzheimer’s Disease, Parkinson’s Disease, and ALS.
Another critical protein for Alzheimer Disease is phosphorylated tau (p-tau), which accumulates in the brain as neurofibrillary tangles. Specific forms of p-tau, such as p-Tau217, are showing remarkable accuracy in detecting amyloid pathology and are increasingly being studied for early detection. Glial fibrillary acidic protein (GFAP) is another important marker, signaling glial reactivity and astrocytic activation, which are common in inflammatory processes associated with neurodegeneration. The analysis of these proteins, along with other markers forming a complex protein signature, is crucial for diagnosis and monitoring.
Why Biomarkers Are Essential for Therapeutic Strategies and Clinical Trials
The impact of biomarkers extends far beyond simple diagnosis; they are fundamental to the advancement of therapeutic strategies and the success of clinical trials. In therapeutic development, biomarkers are essential for identifying individuals most likely to benefit from a particular drug and for monitoring their response to treatment. This precision in patient selection is crucial for maximizing the chances of trial success and for developing therapies that are tailored to an individual’s specific disease pathology. For example, knowing a patient’s specific tau or amyloid profile can guide the choice of investigational treatments. Furthermore, biomarkers can serve as surrogate endpoints in clinical trials, providing an objective measure of treatment efficacy that can sometimes be assessed more quickly than clinical outcomes, thereby accelerating the delivery of new therapies to patients. They also help track disease progression and the impact of treatments, enhancing the management of neurodegenerative disorders.
Breakthroughs in Fluid Biomarkers: Paving the Way for Accessible Diagnostics
The search for accessible and non-invasive diagnostic tools has long been a priority in neurodegenerative disease research. Recent breakthroughs in fluid biomarkers, particularly those derived from blood, are transforming this landscape. These advancements are making it possible to detect disease pathology more easily and affordably, opening new avenues for widespread screening and early detection. The ability to perform routine blood tests for complex neurological conditions represents a paradigm shift, moving diagnostics from specialized centers to primary care settings. This accessibility is vital for managing the growing global burden of neurodegenerative conditions.
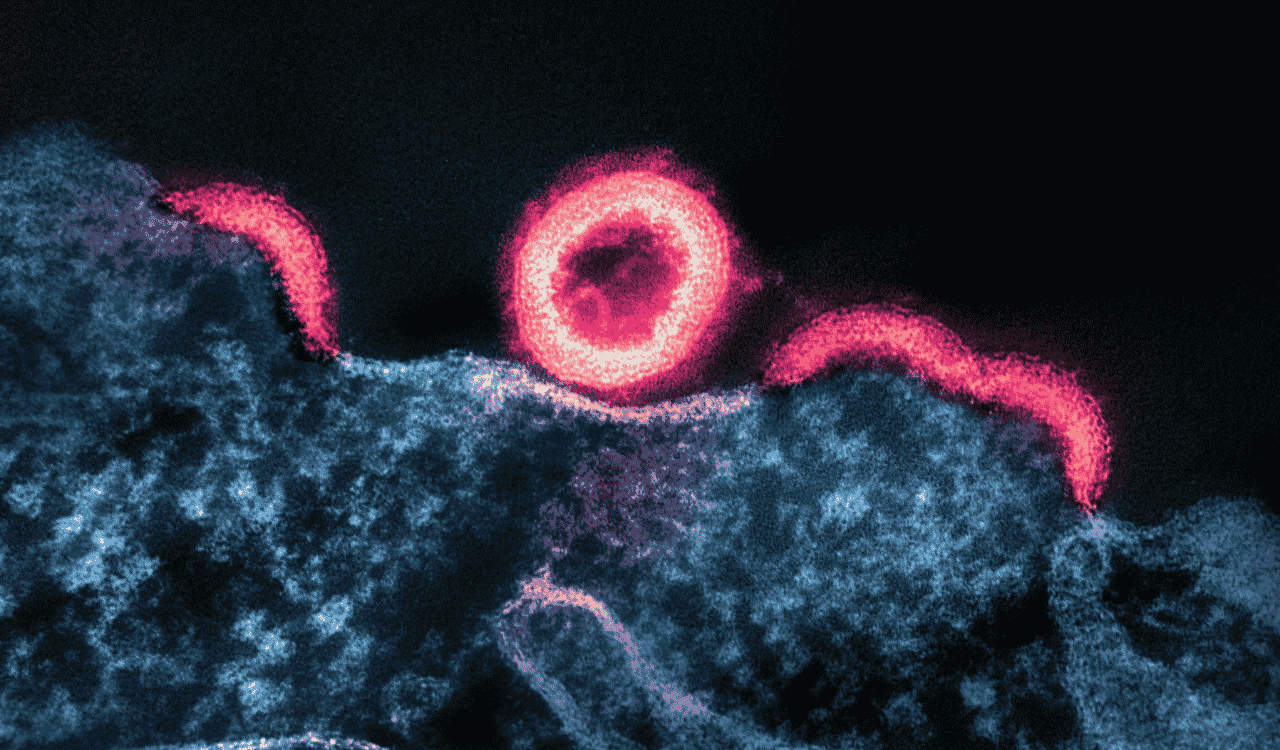
The Rise of Blood-Based Biomarkers: A Game-Changer for Early Detection
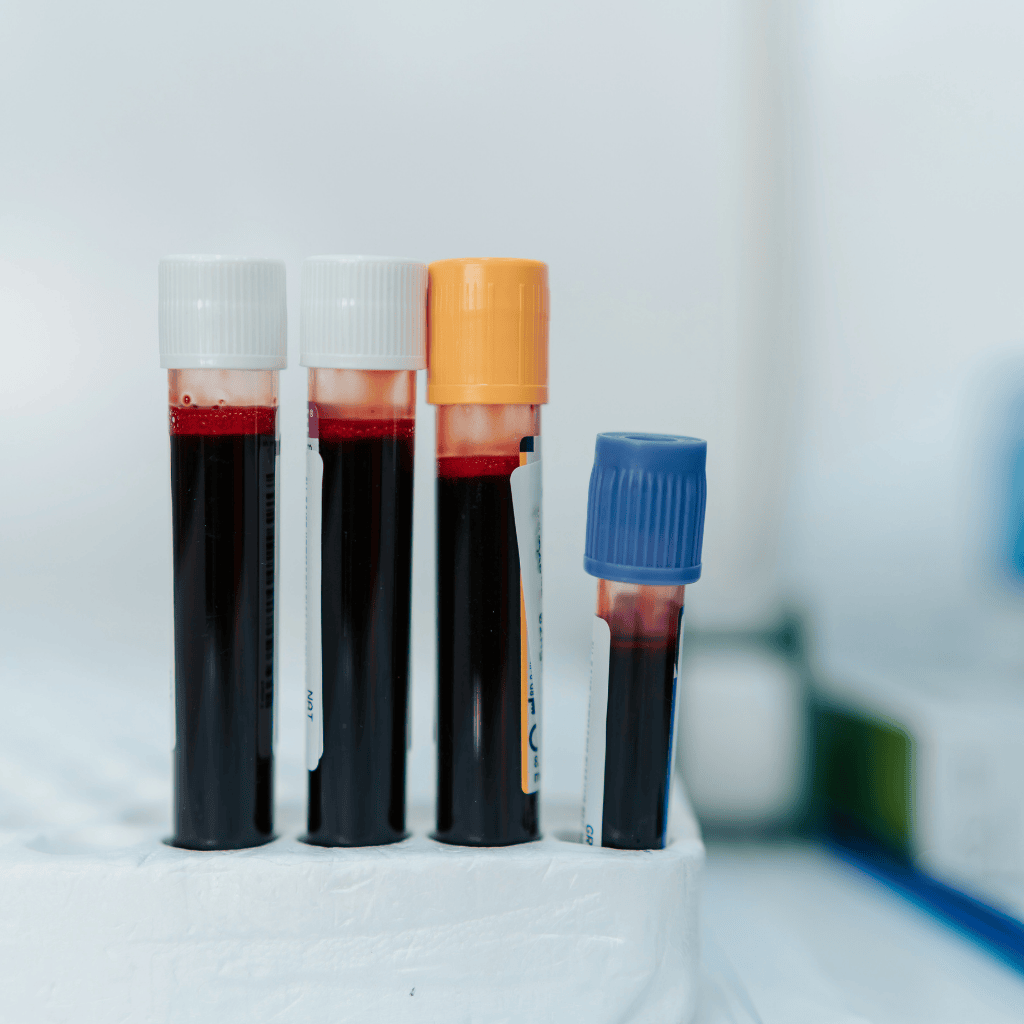
Sensitive detection technologies have propelled blood into the spotlight as a primary source for reliable biomarkers. Blood tests offer a significantly less invasive and more accessible alternative to existing diagnostic methods, making early detection of neurodegenerative diseases more feasible on a large scale. Researchers are now able to detect minute concentrations of specific proteins, such as phosphorylated tau (p-tau) and alpha-synuclein (relevant for Parkinson’s disease), in plasma samples with remarkable accuracy. These blood-based fluid biomarkers are proving to be as accurate as, or even more accurate than, traditional methods like cerebrospinal fluid analysis or PET scans for detecting key pathological hallmarks of diseases like Alzheimer’s disease. The ability to perform regular blood tests could allow for earlier screening, wider treatment windows, and frequent monitoring. Technologies like Dried Blood Collection enable sample collection outside clinics using capillary blood or venous plasma. While blood pressure isn’t a direct biomarker, maintaining healthy levels is crucial for overall brain health and can be an important factor in patient assessment.
Cerebrospinal Fluid (CSF) Biomarkers: The Enduring Gold Standard for Specificity
Despite the promise of blood-based biomarkers, cerebrospinal fluid (CSF) remains vital for specific biomarkers in diagnosing neurodegenerative diseases. Obtained through lumbar puncture, CSF bathes the brain and spinal cord, reflecting the central nervous system’s biochemical environment. For Alzheimer’s disease, CSF analysis of amyloid beta 42 and tau protein is a gold standard for confirming AD pathology. Though CSF collection is invasive and limits screening, it plays a key role in confirming diagnoses and validating blood test findings. Research continues to improve CSF analysis precision. Protein measurements in CSF offer a detailed view of disease state, and understanding the specific brain-derived tau isoforms found in CSF can provide even greater diagnostic specificity.
Unlocking Genetic Insights: The Guiding Star of Genomics in Neurodegenerative Diseases
Understanding the genetic underpinnings of neurodegenerative diseases is providing crucial insights into disease risk, progression, and potential therapeutic targets. Genomics is illuminating individual susceptibilities and informing personalized approaches to care.
The Role of Genetic Risk Factors: Focusing on the APOE ε4 Allele
Genetics plays a significant role in the susceptibility and progression of many neurodegenerative diseases. In Alzheimer’s disease, for instance, the APOE ε4 allele is the strongest known genetic risk factor. Individuals carrying one copy of the APOE ε4 allele have an increased risk of developing AD, while those with two copies have a substantially higher risk and often a younger age of onset. Identifying genetic risk factors like APOE ε4 allows for more precise risk assessment and can inform individuals about their potential predisposition, guiding lifestyle choices and potentially prompting earlier monitoring for disease. This knowledge is invaluable for both research and clinical translation, offering a personalized lens through which to view disease risk. The APOE-e4 gene variant, specifically, affects amyloid beta buildup and clearance, impacting amyloid PET imaging and CSF biomarker accuracy.
How Genetic Variants Influence Biomarker Profiles and Disease Progression
Beyond well-established risk genes like APOE ε4, a vast array of genetic variants can influence the trajectory of neurodegenerative diseases. These variants can impact how proteins involved in disease pathology are produced, processed, or cleared, thereby affecting an individual’s biomarker profiles. For example, genetic differences can alter the rate at which neurofilament light chain is released into the bloodstream or influence the aggregation patterns of tau or alpha-synuclein. Understanding these genetic influences helps explain why individuals with the same disease can present with different clinical symptoms and biomarker levels. This intricate interplay between genetics and biological markers is key to unraveling the complex mechanisms driving disease and developing more targeted therapies.
Neurogenomics and its Impact on Personalized Risk Assessment
The field of neurogenomics combines the study of the nervous system with genomics to understand the genetic basis of neurological disorders. By analyzing an individual’s complete genetic makeup, neurogenomics can identify predisposition to specific neurodegenerative diseases and predict how these diseases might manifest and progress. Individuals with higher genetic risk can make lifestyle changes early. They can watch for early symptoms and consider new treatments or clinical trials. This allows for highly personalized risk assessments, moving beyond broad population-based risk factors. Understanding specific disease-specific genotype data is paramount for developing proactive health strategies.
Beyond Single Markers: The Power of Multi-Omics and Artificial Intelligence
To gain a comprehensive understanding of the intricate biological pathways involved in neurodegeneration, researchers are increasingly employing multi-omics approaches. These strategies integrate data from various molecular levels, including genomics (DNA), transcriptomics (RNA), and proteomics (proteins). By simultaneously analyzing these different layers of biological information, scientists can uncover complex interactions and identify novel biomarkers and therapeutic targets that might be missed when studying each layer in isolation.
For example, correlating genetic variants with specific protein measurements can reveal how genetic predispositions translate into observable biological changes associated with diseases like Alzheimer Disease and Parkinson’s disease. This integrated view provides a more holistic understanding essential for developing effective interventions.
Multi-Omics Approaches: Integrating Genomics, Proteomics, and Transcriptomics
The large, complex data from multi-omics and biomarker studies require advanced tools. Artificial intelligence (AI) and machine learning (ML) help by finding patterns, predicting disease risk, classifying subtypes, and discovering new biomarkers beyond traditional methods. AI also improves clinical trials by selecting patient groups and predicting treatment responses. Platforms like Alamar Biosciences’ NULISA use mass spectrometry and blood-based proteomics to create detailed protein datasets. These platforms enable multiplexed detection of many proteins for detailed profiling.
The NULISAseq CNS Disease Panel 120 helps identify regulatory proteins and glial reactivity markers. Scientists study clinical data, cognitive data, and protein data to build organ age models and calculate protein residuals, helping understand disease severity and organ age gap, crucial for precise therapies. Integrating genomics, proteomics, and transcriptomics reveals the full biological picture, supporting the work of initiatives like the UK DRI and its UK DRI studies.
Artificial Intelligence and Machine Learning: Accelerating Discovery and Prediction
The sheer volume and complexity of data generated by multi-omics studies and biomarker research necessitate advanced analytical tools. Artificial intelligence (AI) and machine learning (ML) are proving invaluable in this regard. These computational techniques can sift through vast datasets to identify subtle patterns, predict disease risk, classify disease subtypes, and even discover novel biomarkers that may not be apparent through traditional statistical methods. AI can also help optimize clinical trial design by identifying optimal patient cohorts and predicting treatment responses. The integration of AI and ML with biomarker discovery is significantly accelerating the pace of research, bringing us closer to effective interventions for neurodegenerative diseases. Analyzing clinical data, cognitive data, and protein data develops organ age models and protein residuals, offering insights into disease severity and organ age gap, key for precise therapies.
From Diagnosis to Precision Treatment: Biomarkers as Therapeutic Guides
The ultimate promise of biomarker research lies in enabling precision therapy. Just as individuals exhibit unique genetic profiles and disease trajectories, their underlying biology can differ. Biomarkers allow clinicians to move beyond generalized treatment approaches and tailor therapies to an individual’s specific disease characteristics.
Enabling Early Intervention: Widening the Therapeutic Window
One of the most significant impacts of advanced biomarker discovery is the ability to enable early intervention. By detecting neurodegenerative diseases in their pre-symptomatic or early symptomatic stages, biomarkers create a wider therapeutic window. This expanded window is critical because many experimental treatments, particularly those aimed at preventing or clearing toxic protein aggregates, are most effective when administered early in the disease course, before substantial neuronal damage has occurred. Early diagnosis facilitated by biomarkers means that individuals can access potentially disease-modifying therapies sooner, offering a greater chance of preserving cognitive function and motor function and improving long-term outcomes. The ability to identify amyloid pathology or primary tauopathies allows for earlier and more targeted interventions.
Guiding Clinical Trials and Therapeutic Responses
Biomarkers are transforming clinical trials for neurodegenerative diseases. They are used to stratify patients, ensuring that participants in a trial have a diagnosis that is consistent with the disease being targeted by the investigational therapy. This precision in patient selection increases the likelihood of observing a treatment effect and reduces the number of participants needed for a trial to achieve statistical significance. Furthermore, biomarkers serve as crucial tools for monitoring treatment response. By tracking changes in specific proteins like neurofilament light chain or markers of amyloid and tau pathology, researchers can objectively assess whether a drug is having the desired biological effect, even before significant clinical changes are apparent.
This makes trials more efficient and guides therapies. Researchers improve biomarkers and use new technologies like mass spectrometry and multiplexed detection methods for earlier diagnosis and better disease management, offering hope and improving millions of lives worldwide. Biomarkers help identify patients who benefit and track responses, boosting success and personalizing therapies.
The Dawn of Precision Therapy: Tailoring Treatments to Individual Profiles
The ultimate promise of biomarker research lies in enabling precision therapy. Just as individuals exhibit unique genetic profiles and disease trajectories, their underlying biology can differ. Biomarkers allow clinicians to move beyond generalized treatment approaches and tailor therapies to an individual’s specific disease characteristics. For example, a patient with Alzheimer’s disease whose biomarker profile indicates a high burden of amyloid plaques might be better suited for an anti-amyloid therapy, while another patient with elevated tau pathology might need a different treatment. Using a patient’s unique biomarker profile helps tailor treatment. This can make treatments work better, reduce side effects, and improve life quality for people with neurodegenerative disease. Understanding synapse function and neural connections through detailed biomarker analysis is key to developing these individualized approaches.
The Collaborative Engine: Accelerating Progress in Neurodegenerative Disease Research
The complexity and scale of neurodegenerative diseases necessitate a collaborative approach. Large-scale initiatives and data-sharing efforts are proving instrumental in driving forward biomarker discovery and therapeutic development.
The Importance of Large Cohorts and Data Sharing
Tackling neurodegenerative diseases needs teamwork. Groups like the Global Neurodegeneration Proteomics Consortium (GNPC) and the Alzheimer’s Disease Data Initiative (ADDI) show this spirit. They unite researchers, institutions, and funders to share data and study many people. This helps find subtle biomarkers, confirm results, and speed discoveries. Sharing data lets scientists build on each other’s work and avoid repeats. Companies like Johnson & Johnson and Gates Ventures support these efforts, working with groups like the Michael J. Fox Foundation and Alzheimer’s Association. The Parkinson’s Progression Markers Initiative (PPMI) is another key example. Analyzing clinical data, cognitive data, and protein data from these large cohorts develops organ age models and protein residuals, offering insights into disease severity and organ age gap, crucial for precise therapies. The Alzheimer’s Disease Data Initiative’s AD Workbench is a prime example of a platform facilitating such collaborative data analysis.
Standardization Efforts for Biomarker Testing and Protein Measurements (Gothenburg, Alzheimer’s Association)
Standardization is very important. It helps turn biomarker discoveries from research labs into regular medical use. This allows doctors worldwide to diagnose and monitor treatment accurately and consistently. Efforts by organizations and research hubs, such as those in Gothenburg and by the Alzheimer’s Association, are focused on establishing standardized protocols for Biomarker Testing and protein measurements. This includes developing and validating assays for specific analytes like p-tau and neurofilament light, ensuring that results are comparable across different laboratories and research settings. Standardization is essential for the successful translation of biomarker discoveries from research laboratories into routine clinical practice, allowing for consistent and accurate diagnoses and therapeutic monitoring.
The Road Ahead: Challenges and Future Directions
While remarkable progress has been made, the journey toward revolutionizing neurodegenerative disease diagnosis and treatment is ongoing. Several critical challenges and exciting future directions lie ahead.
Clinical Translation and Regulatory Approval: Bridging the Gap from Lab to Clinic
A significant hurdle remains in translating promising biomarker discoveries from the research setting into routine clinical practice. This involves rigorous validation studies, establishing assay robustness, and navigating the complex regulatory approval processes of bodies like the FDA. Ensuring that new diagnostic tests are accurate, reliable, and clinically useful requires substantial investment and time. Bridging the gap between the laboratory and the clinic is essential to ensure that patients can benefit from these scientific advancements in a timely manner. The ongoing work in standardizing tests and demonstrating their utility in real-world clinical scenarios is crucial for this translation. The UK DRI (UK Dementia Research Institute) and UK DRI studies are contributing significant research toward this goal.
Addressing Cost-Effectiveness and Global Accessibility
For biomarker diagnostics to truly revolutionize care for neurodegenerative diseases, they must be cost-effective and globally accessible. While blood tests offer a more accessible option than PET scans or cerebrospinal fluid analysis, the cost of developing, manufacturing, and distributing these tests needs to be managed to ensure they can be implemented broadly, even in resource-limited settings. Furthermore, ensuring equitable access to these diagnostic tools, regardless of geographic location or socioeconomic status, is a critical ethical imperative. Initiatives that focus on developing affordable diagnostic platforms and training healthcare professionals globally will be vital for achieving widespread impact. Platforms like the AROG HT System at Crestwood Medical Center aim to make advanced diagnostics more accessible.
Ethical Considerations in Biomarker Testing and Genetic Risk Disclosure
The increasing ability to identify disease predisposition through genetic testing and biomarker analysis raises important ethical considerations. Issues surrounding informed consent, the disclosure of genetic risk information, data privacy, and the potential for psychological distress need to be carefully addressed. Strong ethical guidelines and comprehensive genetic counseling are essential to ensure that biomarker technology advances responsibly and ethically, protecting patient well-being and choice. Patients must be empowered with clear, understandable information about what biomarker testing entails, what the results mean, and the implications for their future health and that of their families. Establishing robust ethical guidelines and providing comprehensive genetic counseling are paramount.
Conclusion
The fight against neurodegenerative diseases like Alzheimer’s Disease and Parkinson’s disease is entering a new era, driven by revolutionary biomarker discoveries. The shift from symptom-based diagnosis to objective, molecular indicators, particularly in easily accessible blood samples, promises early detection, more accurate diagnoses of various dementias and other conditions, and a profound impact on treatment strategies. The integration of proteomics, genomics, and advanced AI is accelerating our understanding of complex neurodegeneration pathways and enabling personalized approaches. NfL, GFAP, and specific tau protein measurements are emerging as crucial markers, while platforms like NULISA and the SomaScan platform are enabling sophisticated blood-based proteomics.
While challenges in clinical translation, cost, and ethical considerations remain, the collaborative efforts of researchers and consortia worldwide, including the Global Neurodegeneration Proteomics Consortium and initiatives supported by the Alzheimer’s Association and the Michael J. Fox Foundation, are building a robust foundation for the future.
The continuous refinement of biomarkers like neurofilament light chain, tau protein, and amyloid beta 42, coupled with advances in mass spectrometry and multiplexed detection methods, offer hope for earlier diagnosis, better monitoring, and improved outcomes. Understanding glial reactivity, astrocytic activation, and microglial activation through detailed protein signature analysis paves the way for targeted therapies, and concepts like organ age models offer deeper insight into disease progression. Biomarker innovation is transforming science and lives by guiding management and the potential for cures for these devastating diseases.




Leave a Reply