Introduction
Alzheimer’s disease, a progressive neurological disorder, has become an increasingly prevalent and concerning issue in today’s aging population. Named after Dr. Alois Alzheimer, who first described the condition in 1906, this disease presents a complex web of challenges for both individuals and their families. Characterized by cognitive decline, memory loss, and impaired reasoning, Alzheimer’s affects the individual’s quality of life and places a significant burden on caregivers and healthcare systems. This comprehensive guide will delve into the intricacies of Alzheimer’s disease, exploring its causes, symptoms, diagnosis, treatment options, and potential preventive measures.
The causes of dementia can vary depending on the types of brain changes that may be taking place. Other forms of dementia include Lewy body dementia, frontotemporal disorders, and vascular dementia. It is common for people to have mixed dementia — a combination of two or more types of dementia. For example, some people have both Alzheimer’s and vascular dementia.
Understanding Alzheimer’s Disease
1. The Neuroscience Behind Alzheimer’s Disease
At its core, Alzheimer’s disease is a neurodegenerative disorder primarily affecting brain cells, particularly neurons, and the intricate networks they form. The brain’s intricate architecture relies on the seamless communication between neurons through synapses, which transmit signals essential for memory, learning, and cognitive function. However, in Alzheimer’s disease, these vital connections begin to deteriorate, leading to characteristic cognitive decline.
The hallmark of Alzheimer’s pathology is the accumulation of abnormal protein aggregates, particularly beta-amyloid plaques and tau tangles. Beta-amyloid, a protein fragment, forms plaques that disrupt communication between neurons and cause inflammation. Tau proteins, on the other hand, accumulate inside neurons, causing them to become tangled and lose their proper functioning. This duo of beta-amyloid plaques and tau tangles severely disrupts brain cell communication and function, ultimately leading to cognitive impairment.
2. Risk Factors and Causes
While the exact cause of Alzheimer’s disease remains elusive, researchers have identified several risk factors that may contribute to its development. Advanced age is the most significant risk factor, with the risk doubling every five years after age 65. Genetic factors also play a role, particularly mutations in genes such as APOE, which are associated with increased risk.
Lifestyle factors such as diet, exercise, and cognitive engagement also influence the risk of developing Alzheimer’s disease. Cardiovascular health, for instance, is closely linked to brain health, and conditions like high blood pressure, high cholesterol, and diabetes can increase the risk. Additionally, a sedentary lifestyle and a lack of mental stimulation may contribute to cognitive decline.
3. Recognizing the Symptoms
The symptoms of Alzheimer’s disease develop gradually and worsen over time. Early signs often involve memory loss, such as forgetting recent conversations, appointments, or where items are placed. As the disease progresses, individuals may experience difficulty with language, problem-solving, and spatial awareness. Personality and mood changes are also common, leading to irritability, anxiety, and depression.
Caregivers and family members should be aware of these changes and seek medical evaluation if they notice persistent cognitive decline. Early diagnosis allows for better management of the disease and implementation of interventions that may slow its progression.
Stages of Alzheimer’s Disease
1. Early-Stage Alzheimer’s
In the initial phase of Alzheimer’s, individuals start to face an increase in memory lapses and other cognitive issues. Challenges may arise with orientation, such as getting lost easily, and with financial tasks like managing finances or settling bills. They may ask the same questions repeatedly, take more time to finish everyday activities, and exhibit changes in personality and behavior. Diagnosis often occurs at this stage.
2. Intermediate-Stage Alzheimer’s
During the intermediate phase, the brain undergoes further deterioration, particularly affecting regions responsible for language, logical thinking, conscious reasoning, and sensory processing, such as accurately identifying sounds and scents. There’s a marked increase in memory loss and confusion, leading to difficulties in recognizing close relatives and friends. Learning new things becomes harder, complex multi-step activities such as dressing become problematic, and adjusting to new circumstances grows increasingly challenging. Additionally, individuals may experience hallucinations, delusions, paranoia, and act impulsively.
3. Advanced-Stage Alzheimer’s
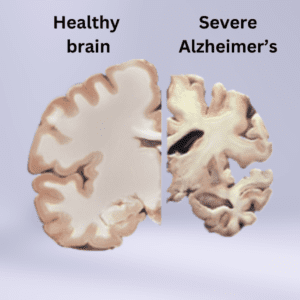
In the final stage of Alzheimer’s, the brain is extensively damaged as plaques and tangles proliferate, and there is a significant reduction in brain tissue. At this advanced stage, individuals lose the ability to communicate and rely entirely on others for their care. As the end of life approaches, they may spend most or all of their time in bed as their body’s functions begin to cease.
Diagnosis and Management
1. Diagnosing Alzheimer’s Disease
Diagnosing Alzheimer’s disease involves a comprehensive assessment of an individual’s medical history, cognitive function, and physical health. Doctors often use various cognitive tests to evaluate memory, thinking, and problem-solving abilities. Imaging techniques like MRI and PET scans may also be employed to visualize brain changes associated with Alzheimer’s pathology.
It’s important to note that diagnosing Alzheimer’s disease can be challenging, as its symptoms overlap with other cognitive disorders. A definitive diagnosis is often only possible through post-mortem examination of brain tissue. However, imaging and biomarker research advancements are improving early detection and accuracy.
2. Treatment Approaches
As of now, there is no cure for Alzheimer’s disease, but various treatment approaches aim to manage symptoms and enhance the quality of life for both individuals with the disease and their caregivers. Treatment plans are tailored to each individual and may include:
Medications: Cholinesterase inhibitors and memantine are commonly prescribed to manage cognitive symptoms and improve memory and thinking. These drugs work by regulating neurotransmitters in the brain.
- Beta-amyloid reduction drugs, such as Aducanumab and Leqembi. Aducanumab has been developed with the aim of addressing and eliminating particular variants of beta-amyloid that amass into formations known as plaques. These accumulations have the potential to play a role in the demise of cells and the depletion of tissue in regions of the brain that hold significant importance for functions such as memory, cognition, learning, and behaviors. Although the brain continues to generate beta-amyloid, aducanumab serves to diminish its quantity. This reduction in beta-amyloid levels could additionally enhance the efficiency of other cognitive processes within the brain.
Lifestyle Modifications: Engaging in regular physical exercise, adopting a brain-healthy diet (rich in fruits, vegetables, whole grains, and lean proteins), and staying mentally active through puzzles, games, and social interactions can positively affect cognitive function.
Behavioral Interventions: Strategies to manage challenging behaviors, such as agitation and aggression, are essential for caregivers. These interventions often involve creating a structured routine, minimizing environmental stressors, and providing sensory stimulation.
3. Ongoing Research and Future Directions
The field of Alzheimer’s research is dynamic and ever-evolving. Researchers continually seek a deeper understanding of the disease’s underlying mechanisms, explore novel treatment approaches, and investigate potential preventive strategies. Promising areas of research include:
Immunotherapy: Researchers are exploring using antibodies to target and clear beta-amyloid plaques and tau tangles. Clinical trials for potential immunotherapies are underway, although challenges related to safety and efficacy remain.
Precision Medicine: Tailoring treatment plans based on an individual’s genetic makeup and biomarker profiles holds promise for more effective interventions. Personalized approaches could lead to better outcomes and more targeted therapies.
Lifestyle Interventions: The role of lifestyle factors in Alzheimer’s prevention and management is gaining traction. Further research is needed to elucidate the specific impact of diet, exercise, sleep, and cognitive engagement on brain health.
Preventing Alzheimer’s Disease
While there is no guaranteed method for preventing Alzheimer’s disease, certain lifestyle choices may reduce the risk of cognitive decline. Adopting a brain-healthy lifestyle involves the following:
Physical Activity: Regular exercise, such as aerobic workouts and strength training, can enhance blood flow to the brain and promote the growth of new neurons. Aim for at least 150 minutes of moderate-intensity exercise each week.
Brain-Healthy Diet: Consume a diet rich in antioxidants, omega-3 fatty acids, and vitamins. Emphasize fruits, vegetables, whole grains, lean proteins, and healthy fats. Reduce intake of processed foods, saturated fats, and sugary snacks.
Cognitive Stimulation: Engaging in mentally stimulating activities, such as puzzles, reading, learning a new instrument, or a new language, can help maintain cognitive function.
Social Engagement: Regular social interactions and connections with friends and family can contribute to brain health. Engage in group activities, join clubs, or volunteer in the community.
Quality Sleep: Prioritize sleep and establish a consistent sleep schedule. Poor sleep can impair cognitive function and increase the risk of cognitive decline.
Conclusion
Alzheimer’s disease remains a complex puzzle with many pieces yet to be fully understood. Its profound impact on individuals, families, and societies underscores the urgent need for continued research, improved diagnostics, and effective treatments. As science advances and our understanding deepens, we move closer to unraveling the mysteries of Alzheimer’s disease and providing hope for those affected by this devastating condition. By embracing brain-healthy lifestyles and supporting ongoing research efforts, we contribute to a future where the burden of Alzheimer’s disease is alleviated, and individuals can age with dignity and vitality.
