Biomarkers as Game-Changers in Neurodegenerative Disease Diagnostics

Imagine a future where the onset of Alzheimer’s or Parkinson’s disease could be predicted and effectively treated before symptoms even appear. Neurodegenerative diseases have long remained shrouded in a veil of uncertainty, with definitive diagnoses often coming too late to alter their devastating trajectories. Biomarkers are the beacons of hope in this landscape, potentially revolutionizing the way neurodegenerative diseases are diagnosed. They give us vital clues about what is happening inside the brain long before outward symptoms manifest. This article delves into the transformative role of biomarkers in neurodegenerative disease diagnostics, providing insights into the current challenges, technological advances, and future perspectives.
Why Biomarkers are Important in Neurodegenerative Disease Diagnostics
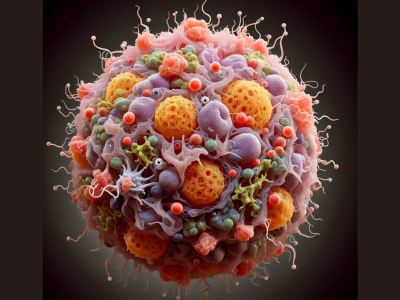
The quest for understanding and managing neurodegenerative diseases has led to a pivotal focus on using biomarkers in diagnostics. Biomarkers are biological indicators that can be measured accurately and reproducibly. In the realm of neurodegenerative disorders—conditions characterized by the gradual degeneration of nerve cells leading to cognitive impairment, behavioral changes, and difficulties with movement—biomarkers provide a window into the brain’s workings and pathological alterations.
In neurodegenerative disease diagnostics, biomarkers like Aβ (Amyloid beta) and tau PET (positron emission tomography) imaging have surfaced as essential tools. They facilitate the detection of regional abnormalities within the brain in vivo, even before noticeable brain tissue loss or atrophy occurs. This early detection is invaluable as it offers potential for interventions before the disease causes irreversible damage.
Furthermore, fluid biomarkers, such as the neurofilament light chain (NfL) levels in cerebrospinal fluid, have proven to be significant. Their correlation with cognitive status and brain atrophy makes them important indicators in clinical trials. However, it’s noteworthy that while such biomarkers reflect neuronal damage, they do not point directly to the specific underlying proteinopathy, such as the presence of neurofibrillary tangles.
The rise of biomarkers as diagnostic tools coincides with the need for enhanced accuracy in identifying neurodegenerative diseases. The biological profiling of these conditions has garnered momentum due to the complex nature of neurological disorders, coupled with strides in genomic and proteomic research. This has expanded the neurodiagnostics market with more refined and targeted diagnostic approaches.
Understanding Neurodegenerative Diseases
Neurodegenerative diseases are the consequence of progressive brain cell loss, resulting in diverse and disruptive symptoms ranging from memory loss and cognitive decline to uncontrollable movements and altered behavior. In the landscape of global health, these conditions represent a growing challenge. For instance, neurodegenerative diseases affected over half a million Canadians in 2016, and with the inevitability of an aging population, these numbers are projected to increase.
Effective treatments to significantly halt or slow the progression of these diseases are currently lacking, underscoring the sheer importance of precise diagnosis for better management and care. Research platforms such as the Ontario Neurodegenerative Disease Research Initiative (ONDRI) have dedicated themselves to understanding the interplay of risk factors and the progression of various neurodegenerative diseases. Conditions like Alzheimer’s disease, frontotemporal dementia, Parkinson’s disease, amyotrophic lateral sclerosis (ALS), and mild cognitive impairment are within their scope of study.
Role of Biomarkers in Disease Diagnosis
The significance of biomarkers for diagnosing neurodegenerative diseases cannot be understated. They have revolutionized the ability to diagnose with accuracy and track the progression of conditions like Alzheimer’s disease and frontotemporal dementia. Aβ and tau PET imaging, for instance, are at the forefront of in vivo diagnostics, allowing clinicians and researchers to observe changes in the brain proactively during clinical trial phases, especially for therapies targeting tau pathology.
Neurofilament light chain (NfL) levels have become important outcome measures in clinical trials due to their association with cognitive decline and atrophy. However, their non-specific nature to a particular proteinopathy reminds us of the complexities at play in neurodegenerative disease diagnostics.
Exosomes, as tiny vesicles present in bodily fluids that facilitate cell-to-cell communication, bring hope as emerging biomarker candidates. Their influence on processes like synaptic plasticity and nerve regeneration could hold keys to understanding and tracking neurological disorders.
Biomarker-based definitions, such as those set by the NIA-AA for Alzheimer’s disease, highlight the shift towards a more informed approach in selecting clinical trial participants. Grounding the definition of Alzheimer’s in measurable biomarkers paves the way for more targeted and effective clinical trial designs.

Types of Biomarkers for Neurodegenerative Diseases
The landscape of neurodegenerative disease research is becoming increasingly sophisticated with the expansion of fluid- and imaging-based biomarkers. These biomarkers serve not just as tools for research but also play a critical role in bridging significant voids in both research and clinical practice. With a growing panel of biomarkers for conditions like Alzheimer’s disease, frontotemporal dementia, and Parkinson’s disease, the possibilities for utilization and interpretation are continually broadening. This panel includes molecular indicators within the blood and cerebrospinal fluid (CSF) and advanced imaging techniques that visualize the brain’s structure and function. Implementing and interpreting such biomarkers are instrumental in advancing neurodegenerative disease diagnostics, promoting a more nuanced understanding of these complex conditions.
Cerebrospinal Fluid Biomarkers
Cerebrospinal fluid (CSF) biomarkers have emerged as pillars in accurately diagnosing Alzheimer’s disease. Notable among these markers are Aβ42, total tau protein, and phosphorylated tau. These specific proteins in the CSF are critical for confirming an Alzheimer’s diagnosis by indicating Aβ and tau positivity—a combination considered indicative of the disease’s hallmark pathologies. The International Working Group’s recommendations for confirmed Alzheimer’s disease diagnoses emphasize the presence of these biomarkers in tandem with specific clinical phenotypes. This CSF biomarker presence solidifies the diagnosis beyond clinical observation alone. Furthermore, the characteristics and trends observed in CSF biomarkers are influential in the development and validation of novel blood-based biomarkers, guiding the pursuit of non-invasive diagnostic techniques with the potential for high diagnostic accuracy.
Blood-based Biomarkers
The paradigm of neurodegenerative disease diagnosis is witnessing a revolution with the advent of blood-based biomarkers. Plasma Neurofilament light chain (NFL), in particular, is a robust indicator that reflects ongoing neurodegenerative processes within the central nervous system, and its presence in the blood plasma correlates closely with CSF NFL concentrations. Blood diagnostics incorporating biomarkers such as plasma NFL are gaining momentum due to their convenience and non-invasive nature. These advances have profound implications for diagnosing a wide array of neurodegenerative diseases, including Alzheimer’s disease (AD), Parkinson’s disease (PD), amyotrophic lateral sclerosis (ALS), frontotemporal dementia (FTD), Huntington’s disease, and Creutzfeldt-Jakob disease (CJD). The precision of blood-based biomarkers in differentiating Alzheimer’s from other conditions aids in prognosis and early diagnosis, potentially enabling earlier intervention for individuals identified as being at risk.
Alzheimer’s disease (AD) is a prevalent cause of dementia that is projected to affect over 78 million people by 2030. Due to limitations in traditional AD biomarkers, there has been a proposal to utilize blood-based biomarkers for diagnosing Alzheimer’s disease. Some machine learning models have shown improved performance in predicting AD by incorporating clinical features into their primary data. This study introduces a machine-learning method for accurately predicting MCI/AD and discovering new blood-based biomarkers (Source: https://www.nature.com/articles/s41598-024-56489-1).
One of the emerging biomarkers in neurodegenerative disease diagnostics is pTau217, a phosphorylated form of tau protein found in cerebrospinal fluid. Studies have shown that elevated levels of pTau217 are associated with Alzheimer’s disease pathology and may serve as a more specific and sensitive marker for the disease compared to other tau proteins. The presence of pTau217 in CSF can aid in early detection and differential diagnosis of Alzheimer’s disease, providing valuable information for patient management and treatment strategies. As research continues to explore the potential of pTau217 as a game-changer in neurodegenerative disease diagnostics, its role in clinical practice is expected to become increasingly significant.
“The strong performance of plasma p-Tau 217 tests is one reason the criteria have been revised,” says Teunissen, who is part of the group tasked with updating the criteria. “Blood biomarkers play a prominent role now.” Lucent Diagnostics, part of Quanterix, recently launched a digital p-Tau 217 immunoassay based on Quanterix’s Simoa (single molecule array) and tau-specific antibodies (Source: nature.com).
Imaging Biomarkers
In the realm of neuroimaging, PET scans wield tracer molecules that facilitate the analysis of proteins associated with neurodegenerative diseases directly from cerebrospinal fluid. In contrast, MRI techniques have established themselves as a fundamental pillar of diagnostic testing, offering clarity in visualizing contrasts between gray and white matter in the brain. Among imaging techniques, Fluorodeoxyglucose (FDG) PET imaging stands out for its use in molecular neuroimaging, critically evaluating neurodegenerative diseases by tracing glucose metabolism patterns. Amyloid PET imaging, endorsed by the US FDA, complements the conventional CSF examination for amyloid-β and tau proteins in the diagnostic process. As ongoing studies continue to validate the clinical utility of amyloid PET imaging, the role and relevance of imaging biomarkers in the diagnostic landscape for neurodegenerative diseases remain pivotal.
Promising Biomarkers for Early Diagnosis of Neurodegenerative Diseases
The advent of biomarkers has brought a seismic shift in the neurodegenerative diseases diagnostics landscape, potentially bridging substantial gaps between research and clinical practice. As neurodegenerative diseases, such as Alzheimer’s, Parkinson’s, and frontotemporal dementia, present with symptoms often when irreversible damage has occurred, the role of biomarkers in early diagnosis is paramount. The array of fluid- and imaging-based biomarkers is ever-expanding, offering the promise of early detection, which, in turn, could revolutionize treatment and patient care. These biomarkers’ evolution and increased utilization have proven essential, calling for accurate implementation and interpretation in both research and clinical settings. With their growing availability and utility in clinical practice, biomarkers are pivotal for advancing our understanding of neurodegenerative diseases and significantly improving the early diagnosis and treatment of these conditions.
Genetic Biomarkers
In the field of neurogenetics, the discovery of genetic biomarkers has shed light on the hereditary nature of many neurodegenerative disorders. Genes such as PSEN1, PSEN2, APP, and C9orf72, GRN, and MAPT, are important genetic indicators for diseases like Alzheimer’s and frontotemporal dementia. A study involving a Colombian cohort has unveiled gene variants linked to neurodegeneration, providing insights into ancestry and genetic admixture. For those families with a history of early-onset dementia and multiple affected first-degree relatives, genetic screening offers a powerful tool for identifying individuals at increased risk. The presence of unique gene variants due to genetic drift in local populations underscores the importance of understanding genetic diversity in the context of dementia, highlighting the potential of genetic biomarkers in personalized medicine.
Fluid Biomarkers
The reliability of fluid biomarkers, particularly in cerebrospinal fluid (CSF), has enhanced diagnostic accuracy for Alzheimer’s disease. The presence of Aβ42, total tau, and phosphorylated tau proteins in CSF are now mainstays in confirming a diagnosis when paired with clinical observations. The pathogenic pathways of amyloid-beta proteinopathy and tau proteinopathy distinguished in CSF have been paramount in understanding the disease’s progression. Moreover, the translation of these insights into the development of blood-based biomarkers such as plasma NFL underscores a transformative step towards non-invasive and highly precise diagnostic tools, cementing their importance in the future clinical landscape.
Imaging Biomarkers
Imaging biomarkers continue to redefine neurodiagnostic protocols with advanced techniques that offer vivid insights into the brain’s structure and function. PET scans using tracer molecules give a direct window into the protein deposits in the cerebrospinal fluid of those with neurodegenerative conditions. In tandem, MRI’s capacity to delineate gray and white matter integrity is paramount to diagnostic testing, supplementing molecular findings with structural insights. By tracing glucose metabolism, the application of fluorodeoxyglucose (FDG) PET imaging underscores the metabolism changes due to neurodegeneration. Furthermore, the FDA-endorsed amyloid PET imaging acts in conjunction with CSF examinations to bolster the accuracy of amyloid-β and tau protein diagnoses. Ongoing research continues to validate these approaches, promising to uphold the robustness of imaging biomarkers in the diagnostic toolkit for neurodegenerative diseases.
Challenges and Limitations of Biomarker Use in Neurodegenerative Disease Diagnostics
The surging interest in biomarkers for neurodegenerative diseases has uncovered challenges and limitations that impede seamless integration into diagnostics. For instance, Frontotemporal Lobar Degeneration (FTLD) biomarkers, synucleinopathies, and other neurodegenerative diseases remain underdeveloped or lack full validation. This uncertainty muddles the quest for a comprehensive biomarker definition for these conditions. Moreover, the debate over which biomarkers can effectively highlight Alzheimer’s disease hallmarks, particularly Aβ and tau lesions, complicates the identification of participants who fit specific biomarker profiles.
Although Aβ load adjustments have been shown in therapeutic trials, correlating these changes with clinical outcomes or neurodegeneration has proved challenging. This disconnect necessitates a cautious approach when considering the implementation of proteinopathy biomarkers in Alzheimer’s disease trials. Given their association with cognitive status and atrophy, fluid markers like neurofilament light chain (NfL) have surfaced as potential trial outcomes. Nevertheless, they lack specificity to distinct proteinopathies and instead reflect a broader landscape of neurodegeneration.
The use of tau PET imaging in tau-focused therapies is growing due to its correlation with cognitive decline and neurodegeneration, which demonstrates potential utility as meaningful clinical trial outcomes. Yet, the complexity of these biomarkers lays bare the pressing need for in-depth understanding and robust methodologies before they can serve as trusted components in neurodegenerative disease diagnostics.
Variability and Heterogeneity of Biomarkers
Biomarkers are invaluable in understanding the intricacies of neurodegenerative disorders. They assist in defining inclusion criteria for clinical trials and monitor disease progression. However, this arena is fraught with variability and heterogeneity among biomarkers, complicating their clinical application. Reliable, non-invasive, cost-effective, and accurate blood-based screening tests are particularly sought to navigate therapy trials’ labyrinth. Promising markers exist, such as the Aβ 1–42 /Aβ 1–40 ratio, Beta-secretase 1 (BACE1) enzyme activity, total tau (t-tau), and neurofilament light (NFL) concentrations.
Yet, the quest for optimal biomarkers is confounded by the influence of biological variables on their detection and quantification. Ensuring that these biomarkers are not only promising but practically applicable requires an exhaustive exploration into their very nature and standardized approaches to their collection, measurement, and data analysis. Only through meticulous standardization can the neurodegenerative disease research community hope to leverage these biomarkers for groundbreaking diagnostics and therapeutic interventions.
Standardization and Validation of Biomarkers
A biomarker’s status is not universally applicable and may only be relevant to certain neuropathological diagnoses. This specificity hints at the complex nature of these markers and cautions against adopting a one-size-fits-all approach. In vivo labeling techniques and high-resolution correlations between biomarkers and neuropathology are indispensable for accurate assessments. Such rigorous validation processes as kinetics quantification or postmortem correlation become essential before these biomarkers are incorporated as inclusion criteria or outcomes in clinical trials.
Validated biomarkers are cornerstones for interpreting the underlying pathology of neurodegenerative diseases. They have the potential to revolutionize early diagnosis, track disease progression, and steer treatment strategies. To maximize their utility in clinical trials, especially in studies directed at disease-modifying therapies, there is a clear mandate for an operational, validated biomarker-based definition for these diseases. This need resonates with the guidelines put forward by the National Institute on Aging and Alzheimer’s Association (NIA-AA) for an in vivo research definition of Alzheimer’s disease, underscoring the necessity for validated biomarkers.
Ethical Considerations and Informed Consent
Ethics take center stage in the realm of biomarker research for neurodegenerative diseases. With research often involving interventions like brain donation, genetic screening, and cerebrospinal fluid collection, there is a profound requirement for written informed consent approved by the Institutional Review Boards (IRBs) such as the one from the Medical Research Institute School of Medicine at Universidad de Antioquia. Publications in scientific literature serve as a foundation for genetic screening practices, while rigorous criteria – such as minor allele frequencies in identified risk-associated variants – enable a more secure interpretation of disease risk.
Standardized protocols assure consistency in neuropathologic assessments of specific genetic mutations, and staining techniques like hematoxylin-eosin maintain scientific rigor. Despite the importance of biomarkers such as cerebrospinal fluid in this research, the invasive nature of collecting this fluid often results in reluctance from both clinicians and patients. These ethical considerations emphasize the need for clear communication and stringent adherence to informed consent practices, ensuring that the rights and well-being of participants are safeguarded throughout the biomarker research process.
The Role of Biomarkers in the Diagnosis and Treatment of Specific Neurodegenerative Diseases
Biomarkers have become instrumental in unraveling the complexity of neurodegenerative diseases. Their ability to detect changes at a molecular level and their application in tracking the progression of these conditions have revolutionized the diagnosis and treatment of cognitive and motor impairment disorders. With biomarkers, clinicians can define more precise inclusion criteria for clinical trials and effectively measure outcome variables. These advancements are particularly evident in the sphere of drug development. For example, neuropathologically validated biomarkers were critical in an amyloid-β immunization trial, showcasing their pivotal role despite the inherent delay due to reliance on postmortem samples.
As new therapeutic approaches emerge, the demand for and significance of biomarkers as diagnostic tools will continue to grow. Various fluid and imaging biomarkers, both in use and in development, demonstrate the dynamic landscape of diagnostic tools that could potentially offer insights into diverse neurodegenerative diseases. Journals like Alzheimer’s Research and Therapy continue to evaluate the utility and potential biases in fluid and imaging biomarkers, emphasizing the need to assess these tools critically for application in neurodegenerative conditions.
Alzheimer’s Disease
In the diagnosis of Alzheimer’s Disease (AD), the structural brain changes can be early harbingers. Imaging studies reveal that brain atrophy, especially in the hippocampus’s presubiculum area, may indicate the initial stages of amyloid-beta (Aβ) accumulation. Remarkably, rare genetic mutations directly impact the amyloid cascade in familial AD cases. These mutations include changes in the amyloid precursor protein (APP), presenilin-1 (PSEN1), and presenilin-2 (PSEN2) genes.
Individuals with trisomy 21 (Down syndrome), who possess an extra APP gene, showcase how genetic factors can influence disease risk, leading to early-onset Alzheimer’s due to increased amyloid production. Modern molecular neuroimaging techniques, such as PET scans that visualize amyloid-β and tau proteins, have become indispensable tools for diagnosing and advancing the understanding of AD. Initiatives like the Alzheimer’s Disease Neuroimaging Initiative harness imaging biomarkers to set benchmarks, categorize disease pathology, and foster clinical study advancements in Alzheimer’s Disease.
Parkinson’s Disease
With an incidence rate of 10–18 occurrences per 100,000 individuals each year in the USA, Parkinson’s Disease (PD) exemplifies a major public health concern. Synucleinopathies, which encompass PD, are characterized by their hallmark α-synuclein aggregates known as Lewy bodies. Beyond these pathologic aggregates, researchers have identified various genetic mutations and environmental factors, like pesticide exposure and traumatic brain injury, linked to the risk of developing PD.
PD can manifest in several ways, from classic PD to PD dementia or dementia with Lewy bodies – all with their own unique spectrum of cognitive, behavioral, and motor symptoms. As the second-most common neurodegenerative condition, PD’s diverse symptomatology underscores the need for a wide range of biomarkers to both diagnose and monitor the progression of the disease.
Huntington’s Disease
Moving to Huntington’s Disease (HD), the detection of biomarkers, such as the [18F]MNI-659 identified through positron emission tomography, offers a novel avenue for early diagnosis. Researchers have noted that concentrations of tau and neurofilament in plasma and cerebrospinal fluid correlate with neurological deterioration in HD. Furthermore, neurofilament light protein detected in blood samples is emerging as a powerful biomarker for neurodegeneration in HD patients.
Epidemiological studies like TRACK-HD harness observational data to analyze predictors of phenotypic progression and disease onset, even in premanifest and early-stage Huntington’s disease. This underscores the utility of biomarkers in not only diagnosis and monitoring of HD but also in enhancing our predictive understanding of disease progression.
Frontotemporal Dementia
The emergence of biomarkers has significantly improved diagnostic accuracy and patient management for frontotemporal dementia (FTD). Biomarkers such as amyloid beta and tau proteins obtained from cerebrospinal fluid or PET scans have reshaped the diagnostic process, following the International Working Group criteria for Alzheimer’s Disease diagnosis. In some instances, patients initially diagnosed with FTD can be recalibrated as cases of atypical AD based on their biomarker profiles, leading to a more precise clinical picture and enhanced outcomes in clinical trials.
Moreover, biomarkers are central to differentiating between behavioral or aphasic syndromes and FTD. Their application aids in the early detection and management of neurodegenerative disorders, facilitating the selection of patients for clinical trials and potentially uncovering the disease in its prodromal stages. The insights gained from biomarker research are not only instrumental in understanding disease progression but also open pathways to innovations in therapeutic interventions.
Current Market Trends in Neurodegenerative Disease Diagnostics
The neurodegenerative disease diagnostics landscape is experiencing transformative growth, driven by advancements in genomics and proteomics. The demand for early and precise diagnostic methods escalates as the age demographic shifts towards an older population. Integration of digital technologies, including smartphones and wearables, has accelerated progress, enabling better prediction, diagnosis, and monitoring of brain disorders. One of the key market trends is the emphasis on accuracy through biological profiling. This involves leveraging systems biology and intricate datasets to uncover the pathophysiology and early diagnostic biomarkers of neurodegenerative diseases. North America remains at the forefront, dominating the global neurodiagnostics market, benefiting from a highly developed healthcare system, high adoption rates of cutting-edge tools, and leading neurodiagnostic device manufacturers.
Neurodiagnostics Market
North America emerged as the market leader for neurodiagnostics in 2018, its dominance supported by its advanced healthcare infrastructure and the rapid adoption of innovative diagnostic tools. Leading market players such as GE Healthcare, Siemens Healthineers, and Philips Healthcare have solidified their positions through product launches and strategic partnerships, driving the expansion of the neurodiagnostics market. As a market highlight, GE Healthcare is commended for its comprehensive range of diagnostic imaging modalities. The global neurological disorder diagnostics market predicts an upward trajectory, expected to reach USD 13,800 million by 2027, guided by a compounding annual growth rate (CAGR) of 4.1%.
Clinical Diagnostic Instruments Market
Clinical diagnostic instruments, including electrodiagnostic tests like EMG and NCV, as well as imaging tests such as CT and MRI scans, form the backbone of neurological disease diagnosis. With a projected market size of USD 13,800 million by 2027, the growth of these instruments is significant. The rising prevalence of neurodegenerative diseases has amplified demand for these clinical diagnostic tools, promoting evaluation and improved management of conditions that affect the nervous system.
Diagnostic Imaging Systems Market
There is a considerable surge in the diagnostic imaging systems market segment, fueled by advancements in MRI, CT, and PET scan technologies. The market is further bolstered by the increasing accessibility of diagnostic centers and hospitals, offering state-of-the-art imaging methods to patients. Notably, this segment is projected to have the highest CAGR among all market segments. The emergence of advanced imaging technologies is significantly improving the visualization and identification of neurological pathologies, thus driving demand for diagnostic imaging systems.
Reagents & Consumables Market
In the European market, Germany claims the largest share, reflecting its prominence in the reagents & consumables sector. Correspondingly, the UK’s growth in neurodegenerative disease incidence is propelling demand for diagnostic reagents & consumables. Japan and India’s markets are also expanding due to increased patient numbers and low entry barriers, respectively. Meanwhile, China’s efforts to upgrade healthcare facilities could potentially surge the market for diagnostic reagents & consumables, taking into account its growing elderly population.
Neurological Disorder Diagnostics Market
The global neurological disorder diagnostics market is expected to flourish, with projections estimating a rise from USD 10,080 million in 2020 to USD 13,800 million by 2027, alongside a CAGR of 4.1%. This market encompasses diverse testing methods crucial for assessing various conditions impacting the nervous system. The US leads the market, propelled by the widespread adoption of advanced diagnostic systems and fertile grounds for R&D. Canada, Germany, and the UK also contribute to market expansion, while Japan and China demonstrate robust growth due to favorable government healthcare initiatives and an increasing patient population. The global landscape for neurological disorder diagnostics is as dynamic as it is promising, indicating a future ripe with innovation and expanded capability in diagnostics.
Future Perspectives and Advances in Biomarker Research
The exploration and identification of effective biomarkers are essential to the evolving field of neurodegenerative disease diagnostics. Pioneers like Kaj Blennow and Henrik Zetterberg are leading efforts to pinpoint previously elusive biomarkers using refined measurement techniques on post-mortem brain samples. These strides lay the groundwork for better diagnosis and understanding of disease pathogenesis.
In recent years, research has zeroed in on promising candidates for specific dementias; for instance, alpha-synuclein for Lewy body dementia and Parkinson’s-like conditions. Plasma neurofilament light chain (NFL) has also attracted attention due to its reflection of neuronal degeneration; providing a potential avenue for universal screening tests for neurodegenerative disorders such as traumatic brain injury, multiple sclerosis, and cerebrovascular disease.
Furthering the compelling list of biomarkers are neural-derived exosome proteins in plasma which are gaining traction as pre-symptomatic indicators of neurodegenerative diseases. These proteins may mirror the CNS neuronal profile, offering a minimally invasive window into the brain’s pathology. Additionally, microRNAs (miRNAs), instrumental in gene expression regulation, have opened new horizons in biomarker research, foretelling a future where diagnostics may focus as much on genetic regulation as on protein misfolding.
Emerging Biomarkers and Technologies
Crafting a detailed understanding of underlying biological processes in neurodegenerative diseases is essential for improving diagnostics. Exosomes—minuscule lipid bilayer vesicles—emerge as instruments of cell-to-cell communication and carry potential as biomarkers when found in various bodily fluids. These carrier vesicles encapsulate snapshots of cellular conditions, including neurological states, making them prime objectives for research.
The field of metabolomics is also projecting a surge with the identification of diverse metabolites. Discoveries like glycerophosphocholine and d-glucosamide have differentiated patients with Alzheimer’s disease from those unaffected, suggesting a powerful diagnostic tool. As technology progresses, specifically through refined nuclear magnetic resonance and mass spectrometry, metabolomics-based biomarkers like 2,4-dihydro butanoic acid show promising correlations with cognitive impairment, marking a significant advance toward early-stage diagnostics.
These explorations usher in a new age for the neurodegenerative diseases diagnostics landscape, providing novel pathways to identify and track disease progression at a molecular level.
Role of Artificial Intelligence in Biomarker Analysis
Artificial intelligence (AI) is reimagining the analytics of biomarkers for neurodegenerative diseases. Machine learning, a subset of AI, has the capacity to increase the reliability of neurocognitive biomarker identification across diverse populations, transcending the variability encountered in individual countries. This sophisticated data processing allows for a refined dissection of complex biological markers and an enhanced predictive power for disease development and progression.
Sophisticated MRI techniques now incorporate AI for heightened diagnostic accuracy. With machine learning, image analysis becomes more astute, picking up subtle visual cues that may precede clinical symptoms. In addition, AI enables a multi-modal, multi-atlas-based approach to detecting neurodegenerative patterns, combining various types of biological and imaging data for a more comprehensive diagnostic picture.
Most importantly, the convergence of AI with biomarker research promises a more accurate and earlier recognition of diseases, vastly improving intervention strategies and patient outcomes. Moreover, this integration streamlines the path to personalized medicine approaches in neurological disorder diagnostics, placing the neurodiagnostics market on a trajectory toward more effective and patient-tailored healthcare solutions.