The Role of Biomarkers in ALS Diagnosis & Monitoring
The Urgency of ALS Research
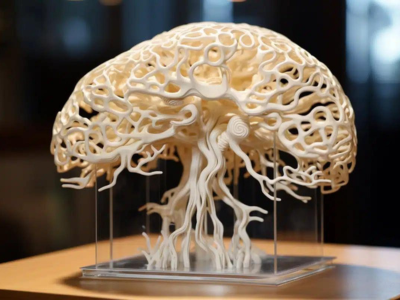
Amyotrophic lateral sclerosis (ALS) is one of the most devastating neurodegenerative diseases. It attacks the motor neurons in the brain and spinal cord, stripping the body of its ability to control movement. Over time, muscles weaken, speech becomes slurred, swallowing becomes difficult, and eventually, the ability to breathe is lost. Most patients live only two to five years after diagnosis.
Despite decades of work, ALS remains without a cure, and current therapies can only modestly slow disease progression. The urgent need for breakthroughs has pushed researchers and drug developers to explore new therapeutic pathways, novel trial designs, and better ways to measure disease activity.
That last point—how we measure ALS—has become a particularly important conversation. And it’s where biomarkers play a critical role.
The Role of Biomarkers in ALS Research
Biomarkers are measurable indicators of a biological process. In ALS, they can help researchers and clinicians:
- Detect the Disease Earlier: Many patients are diagnosed after symptoms become severe, partly because there are no routine screening tools. Biomarkers could help detect ALS activity before significant neuron loss occurs.
- Track Disease Progression: ALS progression is highly variable. Two patients diagnosed at the same time might experience completely different symptom trajectories. Biomarkers can help quantify and monitor these changes objectively.
- Evaluate Treatment Efficacy: In clinical trials, biomarkers can serve as surrogate endpoints—measures that change faster than clinical symptoms and give early signals about whether a drug is working.
Current ALS Biomarkers
Right now, the most studied biomarkers for ALS include:
- Neurofilament Light Chain (NfL): a structural protein released when neurons are damaged.
- Phosphorylated Neurofilament Heavy Chain (pNfH): another neurofilament protein associated with axonal injury.
- TDP-43 Pathology Markers: reflecting the protein aggregates seen in most ALS cases.
- Inflammatory Cytokines: signaling molecules that can be elevated in neurodegeneration.
While these markers have shown promise, they also have limitations. Many are non-specific; they can rise in multiple neurological conditions or even in response to non-neurological injury. For example, NfL can be elevated in traumatic brain injury, Alzheimer’s disease, and multiple sclerosis.
The Problem with Current Biomarker Approaches
ALS biomarker research faces two main challenges:
1. Sample Type Limitations
- Cerebrospinal fluid (CSF) is the gold standard for accessing brain-derived signals. But lumbar punctures are invasive, painful, and carry risks like headaches or bleeding. This makes frequent sampling difficult and can deter trial participation.
- Blood is far easier to collect and is well-suited for large-scale or longitudinal studies. However, it contains signals from the entire body—immune system, muscles, organs—making it hard to isolate brain-specific signals.
2. Specificity vs. Sensitivity
Historically, biomarker work has focused on sensitivity: the ability to detect very low levels of a signal. Sensitivity is still essential, but it’s not enough if you’re detecting the wrong thing.
Take the example of serum NfL. It’s sensitive enough to detect neuronal injury, but it doesn’t tell you where that injury is happening. Is it in the motor cortex? The spinal cord? Somewhere outside the CNS? Without that context, data can be misleading.
In ALS trials, where patient populations are small and the disease is heterogeneous, this lack of specificity can have major consequences:
- False positives that obscure true drug effects.
- Inconsistent results across cohorts.
- Longer, more expensive studies are needed to reach statistical significance.
Why Brain-Specific Biomarkers Matter
Brain-specific biomarkers solve these problems by focusing only on signals that originate in the central nervous system (CNS), specifically, neurons.
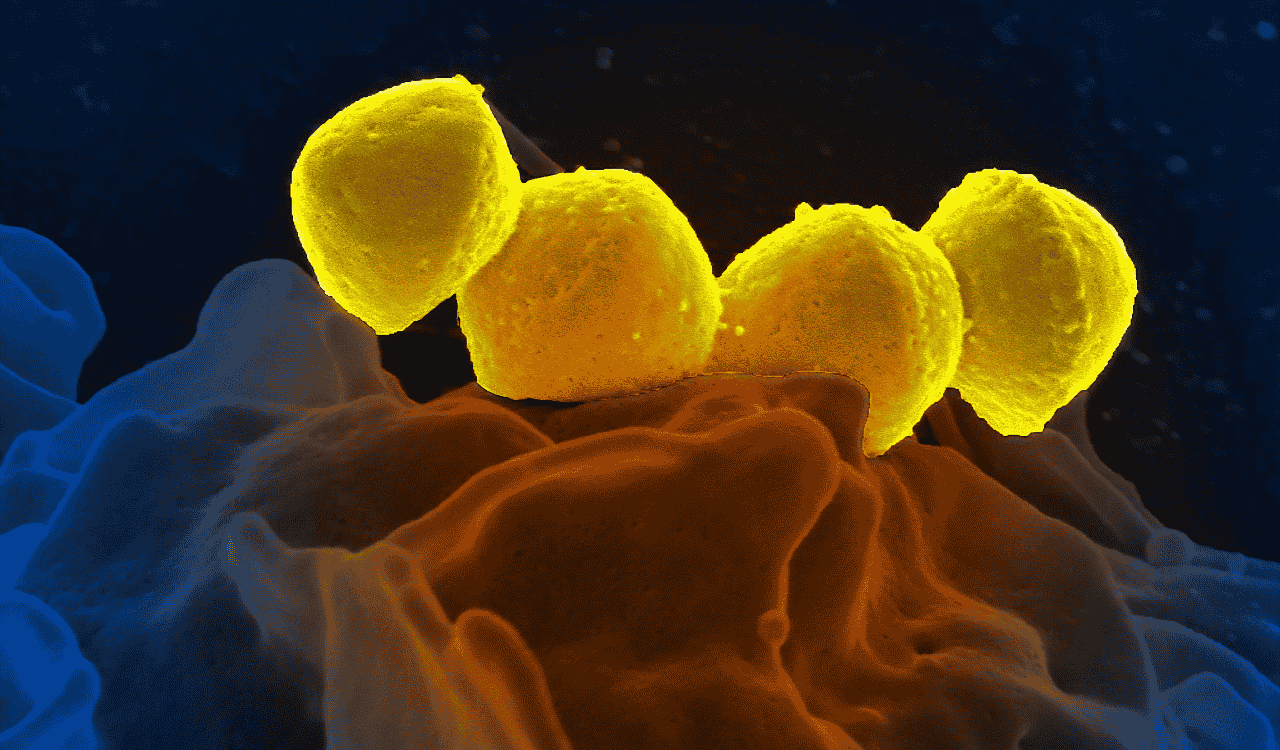
One of the most promising ways to achieve this is through neuron-derived extracellular vesicles (nEVs). These are tiny particles released by neurons into surrounding fluids. They contain proteins, RNA, metabolites, and even fragments of cell membranes that reflect the cell’s internal state.
Think of nEVs as “care packages” sent out by neurons. When isolated from blood, they offer a snapshot of what’s happening in the brain, without the need for an invasive CSF tap.
Why This Matters for ALS
- More accurate tracking: By focusing only on neuron-derived material, researchers can measure true CNS changes without interference from systemic signals.
- Better trial endpoints: Brain-specific biomarkers are more likely to reflect actual disease processes, making them stronger indicators of therapeutic effect.
- Smaller sample requirements: NeuroDex’s isolation method can deliver three validated brain-specific biomarkers from just 25 microliters of plasma, maximizing data from minimal patient burden.
Emerging Techniques for ALS Biomarker Detection
The transition from traditional biomarker detection to neuron-derived vesicle–based methods marks a shift in research priorities:
- From Single Markers to Multiplex Panels: Instead of testing one biomarker at a time, advanced platforms like NeuroDex’s can measure several in parallel from a tiny plasma sample.
- From Raw Sensitivity to Source Fidelity: The goal is no longer just “detect something at low levels,” but “detect the right thing from the right source.”
- From Invasive to Minimally Invasive: NeuroDex’s services and kits make it possible to achieve brain-specific results from small-volume blood samples, opening the door to more frequent and patient-friendly monitoring.
These improvements can:
- Support patient stratification based on biology, not just clinical symptoms.
- Enable real-time monitoring of disease progression in trials.
- Reduce variability, improving statistical power and reducing trial size.
The Road Ahead for ALS Research
ALS research is moving toward a future where specificity and sensitivity work hand-in-hand. In this future, neuron-derived biomarkers from simple blood draws will be key to diagnosing earlier, tracking progression more accurately, and measuring therapeutic impact more reliably.
NeuroDex is helping lead that shift—delivering unmatched neuron-level specificity so researchers can hear the brain, not the noise. For ALS, where every month counts, that clarity can accelerate trials, sharpen decisions, and bring effective therapies closer to patients who urgently need them. Contact us to start the conversation.