Understanding Biomarker Analysis in Medicine
Biomarker analysis is transforming medicine. It offers insights into disease mechanisms and patient responses. This field is crucial for personalized medicine.
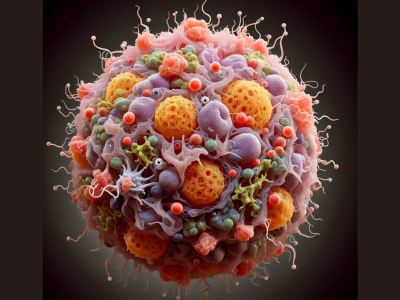
Biomarkers are indicators of biological processes. They can be proteins, genes, or molecules. These markers help in understanding health and disease.
The process of biomarker identification is complex. It involves discovering new markers for diagnosis or treatment. This discovery is vital for medical advancements.
Biomarker detection uses various methods. Imaging, molecular assays, and bioinformatics tools are common. These methods enhance the accuracy of medical diagnoses.
Blood biomarkers are particularly useful. They are easy to obtain and reflect systemic changes. This makes them invaluable in clinical settings.
Biomarker data analysis is essential. It involves statistical and computational methods. These techniques interpret complex biological data effectively.
Biomarker analysis services offer specialized expertise. They provide technology for accurate detection and interpretation. This support is crucial for healthcare professionals.
The field of biomarker analysis is rapidly evolving. It holds significant promise for the future of healthcare. Understanding its intricacies is essential for medical progress.
What Are Biomarkers?
Biomarkers are vital in modern medicine. They serve as measurable indicators of biological states. Through them, we gain insights into health and disease processes.
A biomarker can be many things. It might be a protein, a gene, or another molecule. Each plays a role in signaling normal or abnormal biological activities.
These indicators offer valuable information. They can reveal the presence or risk of disease. Their versatility makes them crucial tools in healthcare.
Not all biomarkers are the same. Some identify disease, while others predict its progression. This diversity is key to understanding their applications.
Common Biomarker Types:
- Proteins: Example includes enzymes and hormones.
- Genes: Genetic markers are widely studied.
- Molecules: Metabolites can indicate health status.
Biomarkers are used in various contexts. They help in diagnosis, monitoring, and treatment decisions. Each application strengthens our understanding of medical conditions.
The discovery of new biomarkers is ongoing. With advances in technology, new markers continue to emerge. These discoveries are essential for advancing personalized medicine.
The Importance of Biomarker Analysis in Medicine
Biomarker analysis is central to personalized medicine. It helps tailor treatments to individual needs. This approach optimizes therapeutic outcomes and minimizes risks.
The role of biomarkers in diagnosis cannot be overstated. They provide early detection of diseases, improving patient prognosis. Early intervention through biomarker use is critical.
Biomarkers guide treatment decisions. They identify the most effective therapies for patients. This targeted approach reduces trial-and-error medication use.
Key Benefits of Biomarker Analysis:
- Personalization: Customizes care for individual profiles.
- Efficiency: Reduces time to effective treatment.
- Accuracy: Enhances diagnosis and monitoring precision.
Monitoring disease progression is another key function. Biomarkers offer real-time insights into disease status. This enables timely adjustments in therapeutic strategies.
Research and drug development are also impacted. Biomarkers identify targets for new drugs. They streamline testing, reducing costs and time. As a result, pharmaceutical development is more efficient and effective.
Types of Biomarkers: Clinical, Diagnostic, Prognostic, and Therapeutic
Biomarkers are diverse tools in medicine. They are classified based on their function and application. This classification includes clinical, diagnostic, prognostic, and therapeutic biomarkers.
Clinical biomarkers evaluate the presence or risk of disease. They are used in routine health screenings. These markers help in measuring normal and abnormal biological processes.
Diagnostic biomarkers play a critical role in disease identification. They enable early disease detection, which is crucial for effective treatment. These biomarkers can confirm or rule out conditions.
Prognostic biomarkers offer insight into a disease’s course. They predict disease progression and potential outcomes. This information helps in planning long-term care strategies.
Therapeutic biomarkers are valuable in treatment selection. They help identify which treatments will likely benefit patients. This reduces unnecessary exposure to ineffective therapies.
Example of Biomarkers in Medicine:
- Clinical: Cholesterol levels for heart disease risk.
- Diagnostic: PSA levels for prostate cancer detection.
- Prognostic: HER2 status in breast cancer.
- Therapeutic: BRCA mutations for cancer treatment planning.
Integration of these biomarkers enhances patient care. Each type brings unique insights to medical practice. Together, they improve diagnosis, treatment, and patient outcomes. This holistic approach is essential for advancing healthcare.
Biomarker Identification: Discovery and Validation
Biomarker identification is a complex process. It starts with the discovery phase. This involves finding new markers that could aid in disease understanding or treatment.
Discovery relies on technology and science. Scientists utilize various methods to pinpoint potential biomarkers. These methods include genomic and proteomic analyses.
Once discovered, biomarkers undergo validation. Validation ensures biomarkers are reliable and reproducible. It confirms that the biomarker consistently indicates the disease or condition.
The validation process involves rigorous testing. Biomarkers are assessed across different populations and settings. This step ensures the biomarker’s clinical relevance and usefulness.
Steps in Biomarker Identification:
- Discovery Phase: Use of advanced technologies to find novel biomarkers.
- Initial Validation: Preliminary testing in controlled settings to assess reliability.
- Reproducibility Testing: Verification across various samples and conditions.
- Clinical Validation: Large-scale testing to confirm clinical utility.

The success of biomarker identification depends on collaboration. Researchers, clinicians, and technologists must work closely. Their combined efforts lead to reliable biomarkers for clinical use.
Biomarker validation is crucial for clinical application. Without validation, biomarkers may not be useful in real-world settings. Careful validation enhances the biomarker’s impact on patient care.
In summary, biomarker identification is a thorough process. Discovery and validation are key phases in this journey. Ensuring accuracy and reliability is essential for their application.
Methods of Biomarker Detection
Biomarker detection is crucial for translating biomarker research into practice. Various methods offer unique advantages in this complex field.
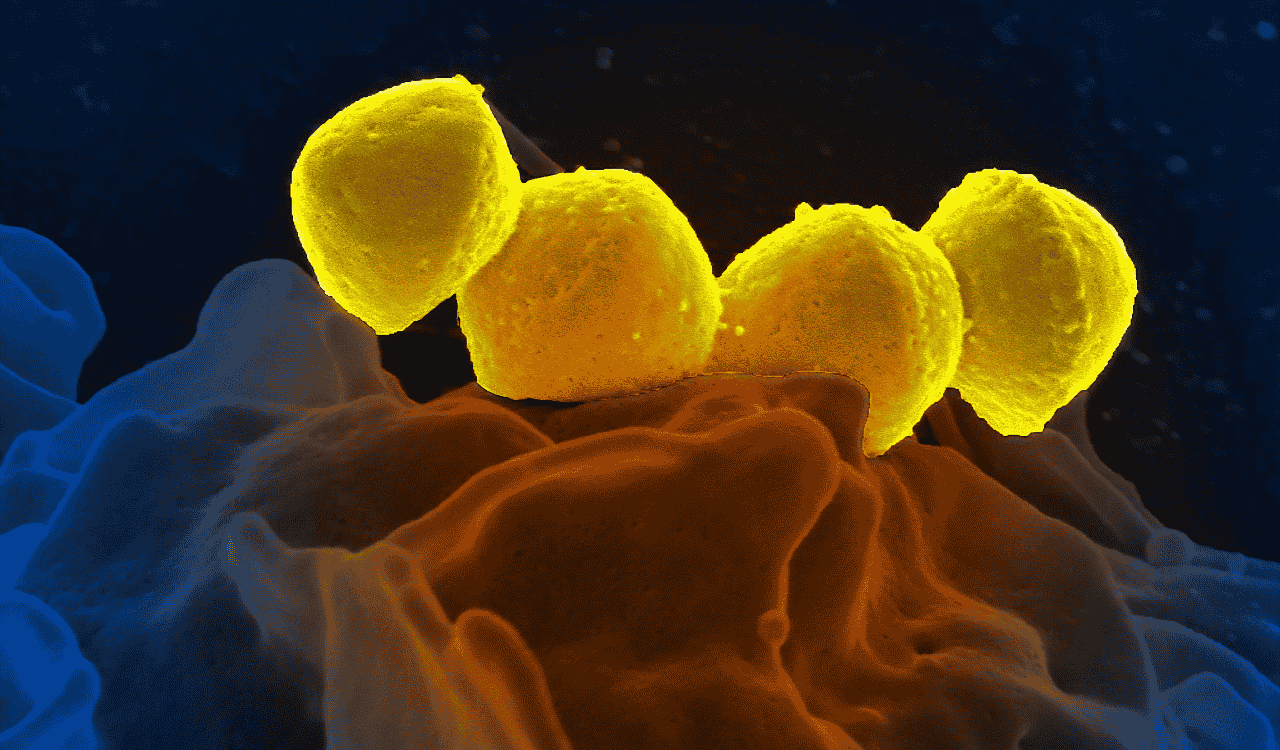
Imaging Techniques: These methods provide visual insights. Imaging allows for the observation of physiological changes. It is often used in oncology to detect tumor markers.
Molecular Assays: These are highly specific and sensitive. They analyze proteins, DNA, and RNA. Techniques such as PCR and ELISA are commonly employed for molecular detection.
Bioinformatics plays a vital role in biomarker detection. Computational tools manage and analyze large datasets. They help identify patterns and correlations among biomarkers.
Mass Spectrometry: This technique is invaluable. It identifies proteins and metabolites in a sample. Mass spectrometry offers precision and depth in biomarker analysis.

Flow Cytometry: It measures physical and chemical characteristics of cells. This method is beneficial for detecting blood biomarkers. It’s widely used in immunology and cancer research.
Next-Generation Sequencing (NGS): NGS technologies accelerate biomarker discovery. They provide comprehensive genomic insights. These insights are essential for personalized medicine.
Common Biomarker Detection Methods:
- Imaging Techniques (e.g., MRI, CT scans)
- Molecular Assays (e.g., PCR, ELISA)
- Bioinformatics Tools (e.g., data analysis software)
- Mass Spectrometry (e.g., protein identification)
- Flow Cytometry (e.g., cell analysis)
- Next-Generation Sequencing (e.g., genomic sequencing)
Each method has its strengths. Choosing the right method depends on the specific biomarker and context. The goal is always accurate and reliable detection.
In summary, biomarker detection is diverse. Methods vary but collectively they advance precision medicine. With technology, the prospects for biomarker detection continue to grow.
Blood Biomarkers: Role and Applications
Blood biomarkers are integral to modern medicine. These markers provide insights into the body’s condition, aiding in diagnosis and monitoring.
The ease of obtaining blood samples makes blood biomarkers highly practical. They reflect systemic changes, serving as excellent indicators of health.
Common blood biomarkers include cholesterol and glucose levels. These are routinely used to assess risk for heart disease and diabetes, respectively.

Blood biomarkers also have applications in oncology. Tumor markers in blood can detect cancer presence and progression, improving management strategies.
Key Applications of Blood Biomarkers:
- Monitoring disease progression
- Assessing treatment responses
- Detecting early signs of diseases
- Evaluating overall health status
In infectious diseases, blood biomarkers identify infections early. This enables prompt treatment, reducing complications. They often guide treatment choices, tailoring interventions to patient needs.
Blood biomarkers offer significant advantages. They allow non-invasive and frequent monitoring of patients, which is less stressful compared to other methods.
With advancements in detection technologies, the potential of blood biomarkers continues to expand. Research is uncovering new biomarkers, enhancing their diagnostic value.
The future of blood biomarkers is promising. As research progresses, these markers will play a larger role in personalized medicine. They have the potential to transform the landscape of disease management.
Biomarker Data Analysis: Tools and Techniques
Biomarker data analysis is pivotal for interpreting complex biological data. It transforms raw data into actionable insights, critical for advancing precision medicine.
The process begins with data collection. This involves gathering information from various sources, such as imaging and assays.
Analysis tools range from basic statistical software to advanced platforms. These tools help in recognizing patterns and correlations within the data.
Common Tools and Techniques in Biomarker Data Analysis:
- Statistical Software: SPSS, SAS
- Bioinformatics Platforms: Bioconductor, Galaxy
- Machine Learning Algorithms: Random Forest, Neural Networks
Bioinformatics plays a crucial role. It employs computational tools to manage and analyze vast datasets, especially in genomics.

Artificial intelligence enhances accuracy. Machine learning algorithms, for instance, identify potential biomarkers faster and more precisely.
Data integration is vital. Combining data from multiple sources provides a comprehensive understanding of biomarker implications.
Despite technological advances, challenges remain. Quality control and standardization across datasets are essential to ensure consistency.
Collaboration is key to successful analysis. It requires interdisciplinary teamwork, merging expertise from biology, data science, and medicine.
Continuous development in analytical techniques promises to improve biomarker data analysis. With technological progress, data interpretation becomes more reliable and meaningful.
Ethical considerations also influence this field. Ensuring data privacy and obtaining informed consent are crucial.
As techniques evolve, biomarker data analysis will become even more influential. It holds the potential to dramatically enhance patient care and therapeutic outcomes. By integrating advanced technology, this process is set to revolutionize how we understand and use biomarker information.
Advances in Biomarker Analysis Technologies
Recent advancements in technology have significantly enhanced biomarker analysis capabilities. These innovations offer improved accuracy and efficiency in identifying and interpreting biomarkers.
Emerging technologies like next-generation sequencing (NGS) have revolutionized genomics. NGS allows for rapid and detailed sequencing of DNA, aiding in the discovery of new biomarkers.
Mass spectrometry has improved protein analysis. It enables precise quantification and identification of proteins, crucial for understanding protein-based biomarkers.
Key Technological Advances:
- Next-Generation Sequencing: Faster and more accurate genome analysis
- Mass Spectrometry: Detailed protein quantification
- CRISPR Technology: Precise gene editing techniques

CRISPR technology is another breakthrough. This gene-editing tool allows precise manipulation of genes, aiding in biomarker research and therapeutic applications.
Artificial intelligence plays a key role. AI and machine learning enhance data analysis by quickly identifying patterns within large datasets.
Robotics and automation streamline laboratory processes. These technologies reduce the time and labor needed for biomarker analysis, increasing throughput and reliability.
Challenges exist alongside these advancements. Integrating new technologies into clinical practice requires validation and standardization processes.
Despite these challenges, technological progress continues to shape the future of biomarker analysis. With these tools, researchers can explore biological complexities more effectively than ever before, paving the way for groundbreaking discoveries in medicine.
Challenges and Limitations in Biomarker Analysis
Biomarker analysis, despite its potential, faces several challenges. These issues can limit its application and effectiveness in clinical settings.
One primary challenge is the variability in biomarker expression. Factors such as genetics, environment, and lifestyle can influence biomarker levels, complicating analysis.
Standardization of testing methods is another concern. Without consistent protocols, results can vary significantly between laboratories, affecting reliability.
Major Limitations in Biomarker Analysis:
- Variability in Expression: Influenced by multiple factors
- Lack of Standardization: Inconsistent methodologies
- Cost and Accessibility: Resources and expertise required

Cost and accessibility are also significant hurdles. Advanced technologies and expertise needed for biomarker analysis can be expensive and are often limited to specialized centers.
Data interpretation poses additional challenges. Biomarker data analysis can be complex, requiring advanced statistical and bioinformatics tools.
Overcoming these challenges is essential for the effective use of biomarkers in medicine. Collaborative efforts and continued research are vital to address these limitations, paving the way for more robust and reliable biomarker applications in healthcare.
Regulatory and Ethical Considerations
Navigating the regulatory landscape is crucial in biomarker analysis. Regulatory bodies ensure that biomarkers used in medicine are safe and effective. This involves rigorous validation processes and compliance with standardized guidelines.
Ethical considerations also play a pivotal role. Researchers must ensure patient consent is obtained before using biomarkers in studies. This transparency is vital for maintaining trust between researchers and participants.
Key Regulatory and Ethical Points:
- Safety and Efficacy: Ensured by regulatory agencies
- Patient Consent: Mandatory for ethical research
- Data Privacy: Protection of personal information is paramount
Data privacy is a significant ethical issue. With the increase in digital data, ensuring the confidentiality of patient information is increasingly challenging. Strict guidelines and secure data systems are necessary to protect patient privacy.
Collaboration among researchers, clinicians, and regulatory bodies is essential. This cooperation ensures that ethical standards are upheld while advancing biomarker research, ultimately leading to safer and more effective medical treatments.
Biomarker Analysis Services: What to Expect
Biomarker analysis services play a crucial role in modern healthcare. They offer specialized expertise and technology necessary for precise biomarker detection and interpretation. These services cater to a wide range of needs, from basic research to clinical trials.
One can expect comprehensive support through every step of the biomarker journey. This includes biomarker discovery, validation, and implementation. Service providers often employ advanced analytical tools to ensure high-quality results.
Features of Biomarker Analysis Services:
- State-of-the-Art Technology: Cutting-edge instruments and methods
- Expert Insight: Access to skilled professionals
- Comprehensive Reporting: Detailed and clear findings
Such services also prioritize customized solutions. By tailoring their offerings to specific client needs, they enhance the effectiveness and efficiency of biomarker projects.

Working with professionals from biomarker analysis services can significantly improve outcomes in both research and clinical settings. They provide critical insights into disease mechanisms, which is invaluable for personalized medicine and drug development.
The Future of Biomarker Analysis in Precision Medicine
Biomarker analysis is expected to revolutionize precision medicine. With its growth, medical treatment can become more tailored, improving outcomes for patients significantly. Future advancements will focus on integrating technology to enhance biomarker efficacy.
Innovative tools like artificial intelligence are already shaping biomarker research. They promise faster and more accurate biomarker identification and interpretation. This transformation will lead to earlier disease detection and better preventive strategies.
Key Future Directions in Biomarker Analysis:
- Integration with AI and Machine Learning
- Enhanced Personalization of Patient Care
- Development of Novel Biomarker Platforms
Biomarkers will likely play a pivotal role in drug discovery. By identifying precise therapeutic targets, they streamline drug development processes. This helps in crafting treatments that are not only effective but also safe.

As biomarker analysis continues to advance, it holds promise for transforming healthcare. We can expect a shift towards more efficient, personalized, and predictive medicine, shaping a healthier future for all.
Conclusion: Key Takeaways and Next Steps
Biomarker analysis is transforming medicine by fostering personalized treatments and enhancing disease diagnosis. This advancement allows for a more precise understanding of individual health profiles. We are witnessing a significant shift towards this technology-driven approach.
The integration of artificial intelligence is particularly noteworthy. It has the potential to streamline biomarker detection and data analysis, making healthcare more efficient. These advancements could drastically alter preventative and therapeutic strategies.
For future progress, collaboration will be essential. Continued cooperation between researchers, clinicians, and industry will accelerate innovations. By embracing these evolving technologies, the medical community can improve patient outcomes and advance towards the next frontier of precision medicine.





Leave a Reply