NeuroDex Pioneers New Multi-Pronged Biomarker for Neurodegenerative Diseases
Rather than a one-size-fits-all blood test that looks for a single pathology, NeuroDex is commercializing a novel scientific approach, based on the study of extracellular vesicles – that can decipher “mixed pathology” in dementia and lead to a more personalized treatment plan.
The Challenge
Whenever we write about a company in the Alzheimer’s Moonshot we have to start by considering where they fall on the care continuum. Are they working on education, early diagnosis, treatment, caregiving? For a long time, there was a lack of funding in early diagnosis because there was little progress on a treatment. Why find out that you have Alzheimer’s if there’s nothing you can do about it? But our treatment paradigm is shifting dramatically, and every week it feels like there is new momentum towards therapies that could slow or stop the disease.
With these therapies comes a renewed interest, and need, for early detection of Alzheimer’s and stratification of the patient population based on the underlying pathology.
It’s been a big year for scientists and researchers working on the diagnosis of Alzheimer’s and other dementias. We’ve seen everything from voice biomarkers to eye tracking. But pretty much everyone agrees that the gold standard would be an accurate blood test that could diagnose Alzheimer’s and detect the underlying pathology.
There have been big Alzheimer’s headlines on the blood-based biomarker front. Blood biomarkers for amyloid and tau pathologies have shown significant promise and are slowly entering the clinical diagnosis process. However, that’s just one biomarker. Pathologies like alpha-synuclein, which occurs in about 30% of dementia patients, and TDP43, which occurs in about 40% of dementia patients, remain without a diagnostic test. Thus, patients receive inaccurate or at least partial diagnoses of their disease.
Erez Eitan, PhD, CSO & Co-founder of NeuroDex, is leveraging years of scientific research to take blood-based biomarkers for Alzheimer’s to the next level. With his team in Boston, Eitan is using a unique biological process in the cells to not only predict Alzheimer’s early, but provide a more precise picture of the person’s pathology, and thus what treatment they should receive.
Origin Story
Every scientist needs a focus. Some love organoids, the organ-like structures that can be grown in a petri dish. Others spend their careers looking at stem cells. For Erez Eitan, the road of scientific discovery has always had one unifying concept: extracellular vesicles.
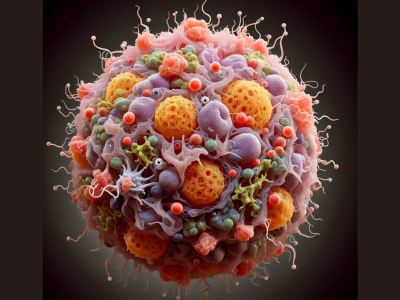
What are extracellular vesicles? They’re extremely tiny “containers” that move between cells performing important functions like transporting material and getting rid of waste.
Eitan “discovered” this area of biology as a neuroscience graduate student in Israel and was immediately hooked. What convinced Eitan that extracellular vesicles were, in his words, “really cool” was the fact that these seemingly insignificant structures carry proteins, RNA, and lipids between cells.
“It completely changes the way we understand intracellular communication,” says Eitan.
Understanding that extracellular vesicles serve as the body’s natural mail system, scientists began to understand that they could read the return address and know where a cell came from.
Practically speaking, that means that by looking at where an extracellular vesicles came from, scientists had access to a highly-specific, powerful, and versatile diagnostic platform.
Eitan was convinced that extracellular vesicles held the potential for many future breakthroughs, so he dedicated his postdoctoral research to the topic and became the first person to study this area of science at the National Institute on Aging.
Eitan’s eureka breakthrough came when he discovered that these vesicles cross the blood-brain barrier and wind up carrying information about the brain. That discovery, Eitan explains, opened up the opportunity to have the “first true liquid biopsy of the brain.” Such a test would enable scientists to understand the pathology in the brain from a simple blood test. Using this technique, he and his team showed that they could detect Alzheimer’s diseases early, years before the onset of symptoms. Moreover, they understood that this technique enables the detection of changes in proteins that are not brain-specific, thus detecting much more information on the brain than just tau and amyloid pathology.
To this point in Eitan’s work, everything lived in the lab, and existed to advance scientific inquiry. But with the discovery of a blood test that provides a window into the brain, Eitan knew that he needed to move out of the lab and into the market. This was a discovery that could change the trajectory of care for millions of people. It needed to be commercialized, which presented a whole new set of challenges.
“There is so much need in the market for a blood test that can detect different brain pathologies, and can monitor therapeutic target engagement,” says Eitan. “It’s not only about early detection of one disease, it’s about really understanding the underlying pathology, what is the driving factor that needs to be treated.”
With that commercialization challenge in mind, NeuroDex was formed in 2018.
Under the Hood
“What we are doing in NeuroDex is developing a blood test for neurological diseases that are based on the isolation of extracellular vesicles that are released by neurons into the circulation,” Eitan explains. “That technology improves the specificity of every biomarker toward changes that occur in the brain at the site of the disease.” NeuroDex isn’t limited to measuring a specific pathology, like some Alzheimer’s blood tests are. They’re diagnosing the core pathology and the “individual signature” of the disease.
Today NeuroDex is taking their scientific discoveries and translating them into an industrial-grade process including automation, quality control, and quality assurance that can be used by pharmaceutical companies to support clinical trials. They already have several pharma and biotech collaborations and are involved in several clinical trials as exploratory biomarkers.
NeuroDex isn’t the only lab working on biomarkers based on extracellular vesicles. Other labs have tried the same thing, but few have succeeded. Why? Eitan says it mainly comes down to persistence and dedication. Extracellular vesicles (EVs) are larger and more complex than proteins and much smaller than cells. Working with EVs requires specific expertise that comes from experience. For Eitan, working with EVs has been a 10+ year project. “I truly dedicated myself to this topic and to develop EV-based immunoassays.”
NeuroDex supports pharmaceutical companies in two main ways. They’ve developed a biomarker product that aids drug discovery, and another that offers a clinical biomarker to improve clinical trials.
Eitan explains that with NeuroDex, clinical trials can be faster and more accurate because better biomarkers lead to more accurate population selection. Also, more accurate biomarkers allow researchers to quickly evaluate treatment responses and know if the drug works. The information the biomarker provides can significantly shift the risk-to-reward ratio of clinical trials. Finally, once a drug gets to market, better biomarkers can help make sure the therapies get to the people who actually need them based on their personal pathology, increasing efficacy and reducing unnecessary side effects.
Final Word
You don’t have to have a PhD in extracellular vesicles to know that Dr. Erez Eitan and the team at NeuroDex are a key part of an exciting wave of innovation in neuroscience. Join us as we proudly welcome them to the Alzheimer’s Moonshot Community. We’ll be tracking their progress through StartUp Health’s various media channels, so stay tuned!
Connect with NeuroDex via email
- Reference: https://www.startuphealth.com/startup-health-blog/neurodex-pioneers-new-multi-pronged-biomarker-for-neurodegenerative-diseases